Cancer Cell:基于多蛋白复合物的癌症精准治疗范式,有望攻克一半以上的肿瘤
2019-11-05 Blake 转化医学网
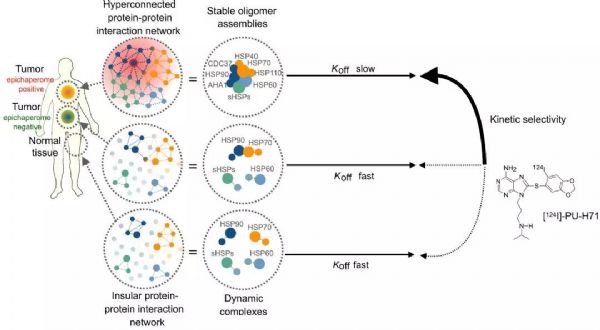
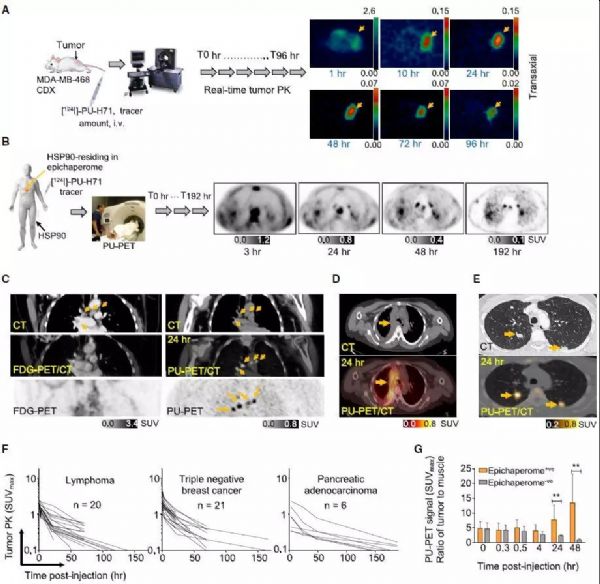
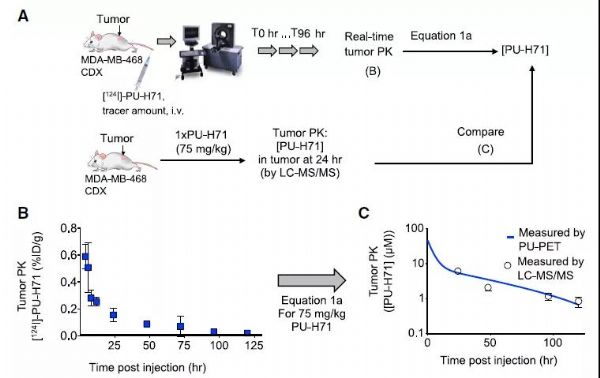
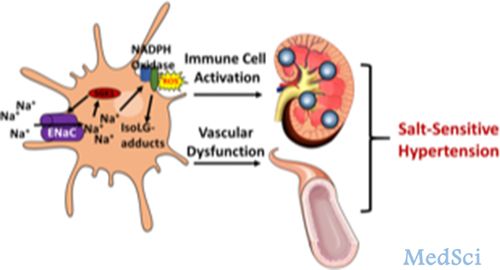
蛋白质是细胞功能的执行者,蛋白互作网络(Protein-Protein Interaction,PPI)通过蛋白之间的相互作用参与基因调节、基因表达、信号传递、代谢及周期调控等各个环节。在肿瘤恶化过程中,细胞中蛋白质互作网络会发生改变,然而,目前并没有针对这种变化的诊断工具。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#cancer cell#
41
#Cell#
33
#CEL#
37
#复合物#
38
#精准治疗#
45
#精准#
30