Dig Dis Sci: 结肠息肉切除术后恢复抗凝的时机和术后并发症的发生率之间的关系
2022-02-26 MedSci原创 MedSci原创
腺瘤性息肉 adenomatous polyp 又称“息肉状腺瘤”。黏膜的腺瘤,多呈息肉状,见于胃肠黏膜,更多在结肠。单发性或多发性,有蒂或无蒂。家族性息肉病患者,结肠黏膜有多个大小不等的息肉状腺瘤。
腺瘤性结肠息肉是结肠癌的前兆,结肠镜下息肉切除术是为了防止此类癌症的发展。不幸的是,息肉切除术与胃肠道 (GI) 出血的风险密切相关,而且医生通常会建议接受抗凝治疗的患者在择期结肠镜检查前停用抗凝剂,但是息肉切除术后恢复抗凝治疗的最佳时间仍然是一个未解决的问题。抗凝恢复过快可能会导致胃肠道出血,而延迟过长可能会导致灾难性的血栓栓塞事件。目前关于结肠镜息肉切除术后何时重新开始抗凝治疗的指南主要基于专家意见而非研究数据。在这项研究中,研究人员探讨了内镜医师在息肉切除术后延迟重新开始抗凝的原因以及息肉切除术后恢复抗凝的时间与延迟性息肉切除术后出血 (PPB) 和血栓栓塞 (TE) 事件之间的关系。
为了完成本项研究,研究人员对早期研究中因息肉切除术而停用抗凝剂的患者进行了事后分析。研究人员比较了临床上重要的延迟 PPB 和 TE 事件与恢复抗凝时间的关系。延迟恢复定义为息肉切除术后> 2天。

研究结果显示在437例患者中,早恢复抗凝治疗的有351例,延迟恢复的有86例。与早期恢复者相比,晚期恢复者的息肉切除复杂性更高。晚期恢复者与早期恢复者的 PPB 率较高(2.3% vs. 0.9%,增加 1.47%,95% CI [- 2.58-5.52],p = 0.26)。TE事件在晚期恢复者比早期恢复者更频繁 [0% VS 1.2% 30天,0% VS 2.3%,95% CI 0.3-8,90天,( p = 0.04) ]。在多变量分析中,重新开始抗凝的时间并不是 PPB 的显着预测因子(OR 0.97,95% CI 0.61-1.44,p= 0.897)。显着的预测因素是息肉直径≥1 cm (OR 4.14, 95% CI 1.27–13.66, p = 0.014) 和电灼技术的使用 (OR 11.43, 95% CI 1.35–80.80, p = 0.014)。
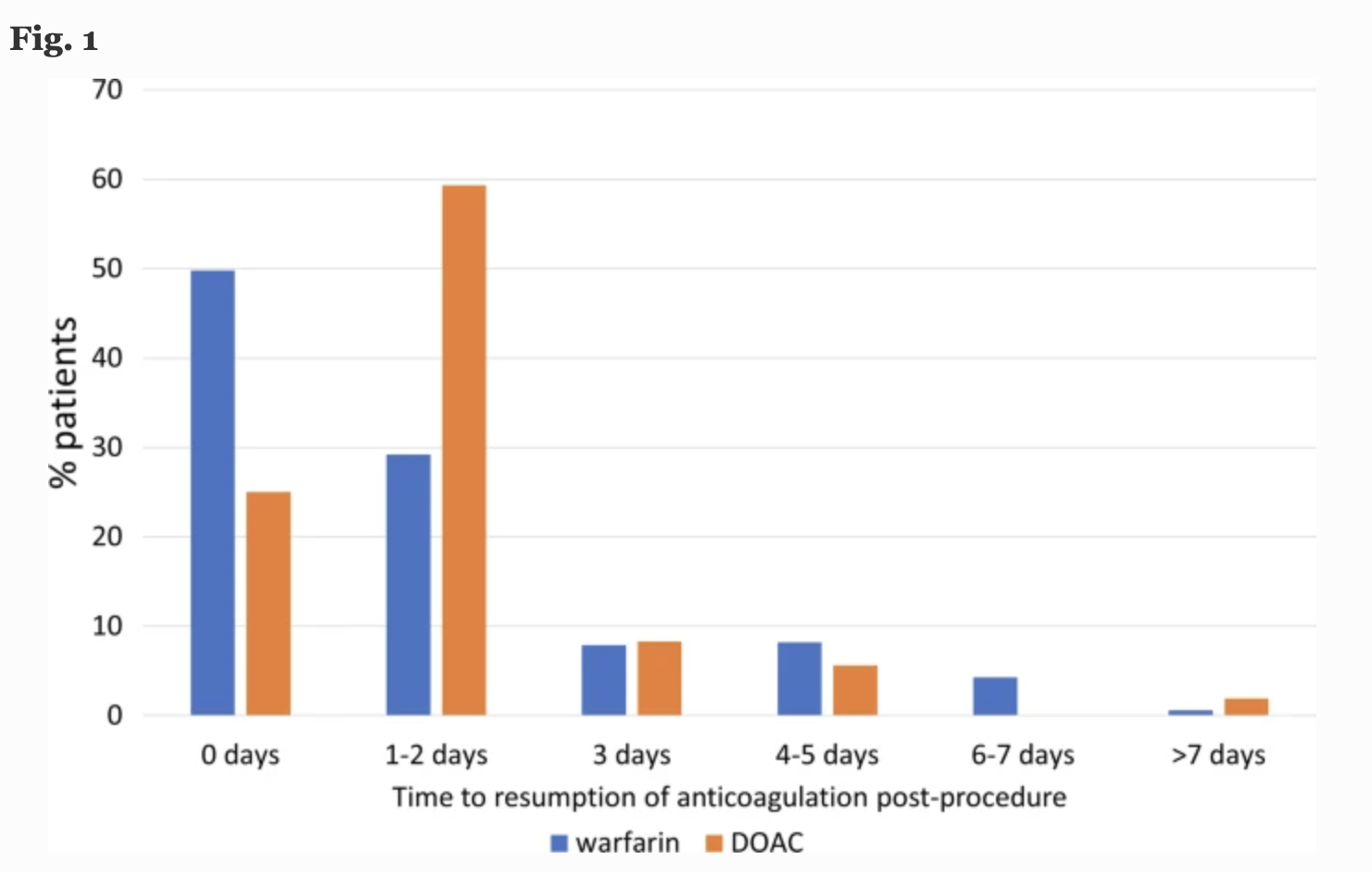
本项研究证实在复杂的息肉切除术后,医生更常延迟抗凝恢复。重新开始抗凝的时间不是 PPB 的重要风险因素,延迟恢复者在 90 天内的 TE 事件发生率显着升高。考虑到 TE 事件的潜在灾难性后果和 PPB 的一般良性结果,临床医生应谨慎对待延迟息肉切除术后恢复抗凝治疗。
原始出处:
Benjamin R. Chebaa. Et al. Timing of Resumption of Anticoagulation After Polypectomy and Frequency of Post-procedural Complications: A Post-hoc Analysis. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
51
#Dis#
27
#发生率#
39
#并发#
49
#息肉切除术#
45