Diabetic Med:喀拉拉邦糖尿病预防计划参与者的基线特征:亚洲印第安人生活方式干预的集群随机对照试验
2017-06-29 MedSci MedSci原创
近日,国际杂志 《Diabetic medicine》上在线发表一项关于喀拉拉邦糖尿病预防计划参与者的基线特征,亚洲印第安人生活方式干预的集群随机对照试验的研究,旨在描述喀拉拉邦糖尿病预防计划参与者的基线特征。
近日,国际杂志 《Diabetic medicine》上在线发表一项关于喀拉拉邦糖尿病预防计划参与者的基线特征,亚洲印第安人生活方式干预的集群随机对照试验的研究,旨在描述喀拉拉邦糖尿病预防计划参与者的基线特征。
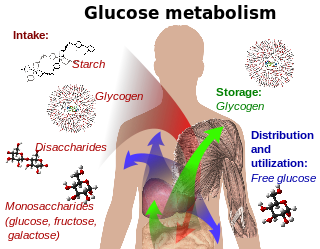
喀拉拉邦糖尿病预防计划是一项生活方式干预用于预防印度2型糖尿病的集群随机对照试验。研究的参与者为30-60岁的印度糖尿病风险评分≥60,口服葡萄糖耐量试验中没有2型糖尿病。使用标准化工具收集人口统计学,生活方式,临床和生化特征数据。
使用印度糖尿病风险评分筛选出2586人,其中1529人(59.1%)得分≥60, 1209例(79.1%)接受口服葡萄糖耐量试验。共有202人(16.7%)未诊断为2型糖尿病,被排除在外,其余1007人参加了试验(对照组,n = 507;干预组,n = 500)。平均参与者年龄为46.0±7.5岁,女性为47.2%。印度糖尿病风险评分平均值为67.1±8.4。超过三分之二(69.0%)患有前期糖尿病,31.0%具有正常的葡萄糖耐量。心脏代谢危险因素的流行程度高,包括烟草使用(男性为34.4%),酒精使用(男性为39.3%),无休闲运动(98.0%),不每天摄入水果和蔬菜(78.7%),家庭糖尿病史(47.9%),超重或肥胖(68.5%),高血压(22.3%)和血脂异常(85.4%)
喀拉拉邦糖尿病预防计划招募参与者使用糖尿病风险评分。参与者中有大部分患有前期糖尿病,心脏代谢危险因素高。该试验将评估基于糖尿病风险评分选择的人群中生活方式干预的有效性。
原始出处:
T. Sathish, B. Oldenburg, R. J. Tapp,et al. Baseline
characteristics of participants in the Kerala Diabetes Prevention Program: a
cluster randomized controlled trial of lifestyle intervention in Asian Indians.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#对照试验#
30
#BET#
32
#DIA#
23
#Diabetic#
29
#对照#
27
#糖尿病预防#
27
#随机对照试验#
23
#Med#
21
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
36
学习了受益匪浅
47