Spine :全美胸椎间盘突出的治疗趋势和并发症
2014-11-12 orthowhq 新英格兰医学杂志
1934年,Mixter和Barr在《新英格兰医学杂志》报道采用椎板切除术治疗三例胸椎间盘突出患者,疗效一般。从此,胸椎间盘突出的治疗历经变革。早期的脊柱外科医生多采用椎板切除减压,常合并严重的致病率和致死率。并发症率高和疗效差,很明显,需更好的手术治疗方法。 20世纪60年代开始,文献中有突破椎板切除减压的新治疗方法。包括前路/侧前路(侧前路开胸、胸腔镜)和后路/后外侧(经椎弓根、经关
1934年,Mixter和Barr在《新英格兰医学杂志》报道采用椎板切除术治疗三例胸椎间盘突出患者,疗效一般。从此,胸椎间盘突出的治疗历经变革。早期的脊柱外科医生多采用椎板切除减压,常合并严重的致病率和致死率。并发症率高和疗效差,很明显,需更好的手术治疗方法。
20世纪60年代开始,文献中有突破椎板切除减压的新治疗方法。包括前路/侧前路(侧前路开胸、胸腔镜)和后路/后外侧(经椎弓根、经关节突保留椎弓根、外侧胸腔外、外侧肩胛旁胸膜外、后外侧肋横突入路)。
1998年,Fessler和Sturgill对胸椎间盘入路进行了综述,椎板切除的致病率为59%,致死率13%,而前路和后外侧入路致病率低。但未前路和后外侧入路致病率的差别。之后又有学者证实前路和后外侧入路致病率相近。
但迄今为止,胸椎间盘突出前路或后外侧入路减压后,是否应行脊柱融合;前路/前外侧入路减压融合(ASF),后路/后外侧减压(PSF)和融合以及单纯椎间盘切除减压(DDE)的疗效比较,均不明确。
美国约翰霍普金斯大学骨科的学者进行了一项大样本数据库的研究,明确了全美胸椎间盘突出的治疗趋势和并发症,文章于2014年9月发表在Spine上。
该研究取样来自美国全国住院患者样本数据库中,2000年至2010年间,因胸椎间盘突出压迫脊髓行脊柱手术的13837例患者,手术类型通过国际疾病分类第九版(ICD-9-CM),临床修订版的手术编码加以界定。对发生静脉血栓栓塞及未发生的患者的一般情况(年龄、性别和保险情况),医院特征(教学地位、床数和地理特征),住院致死率及资源利用情况(住院时间和总费用)特点加以分析。
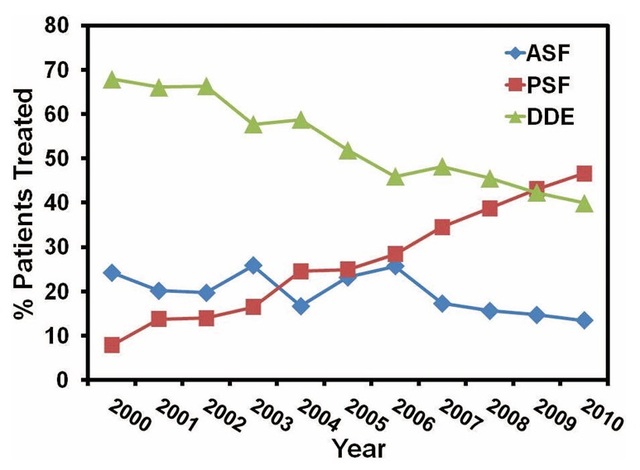
研究结果显示,在研究的区间,胸椎间盘突出的治疗方法,由2000年2/3患者行DDE,逐步变为2010年1/2患者行DDE(图1)。与其它入路组相比,行ASF的患者更为年轻,有私人保险的比率更高。DDE在非教学医院开展的更多。

图1 美国2000年到2010年胸椎间盘突出压迫脊髓患者手术入路的变化趋势。ASF为前路/前外侧减压融合;PSF为后路/后外侧减压融合;DDE单纯椎间盘减压切除,不固定。
ASF并发症率最高(24.2%),特别是肺部和心脏并发症。致死率分别为DDE和PSF的2.8倍和2倍。DDE组的患者住院时间和费用低于其它两个组。
以上结果表明,在过去10年里,胸椎间盘突出压迫脊髓的患者,行PSF的患者明显增多。ASF术后并发症和死亡率最高,DDE患者并发症少,住院周期短,费用低。
本研究明确了胸椎椎间盘突出手术入路在过去十年里的变化趋势,并比较了三种不同入路和治疗方法的功效。总体而言,胸椎间盘突出压迫脊髓,手术并发症率为14.5%,近7%为肺部并发症(绝大多数为ASF患者)。
既往文献中对神经系统并发症探讨不多,本研究中多神经系统并发症定义为:由于手术或手术内置物引起的神经系统并发症,如手术后运动或感觉变化,和围手术期脑血管梗塞或出血。本研究中,胸椎间盘突出手术后,神经系统并发症率为0.5%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Spine#
24
#并发#
32
#椎间盘突出#
33
#胸椎#
0