Neurology:绝经年龄越早,生殖寿命越短(≤35年),女性发生动脉瘤性蛛网膜下腔出血(ASAH)风险就越高!
2022-04-03 Naomi MedSci原创
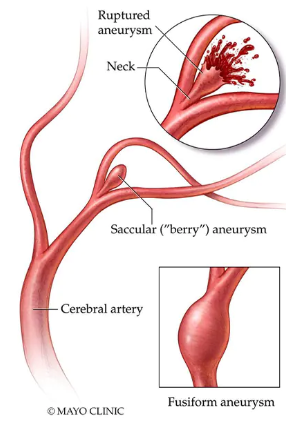
脑动脉瘤破裂导致的动脉瘤蛛网膜下腔出血(ASAH)是一种致死率和致残率都很高的疾病,在绝经后女性中更为常见。近日,研究人员证实,绝经年龄越早,生殖寿命越短(≤为35岁),女性发生ASAH的风险就越高。
脑动脉瘤破裂所致蛛网膜下腔出血是一种致死率和致残率都很高的疾病。与绝经前妇女相比,绝经后妇女动脉瘤性蛛网膜下腔出血(ASAH)和随后的并发症(包括脑血管痉挛)的发生率更高。
尽管目前尚不清楚绝经后妇女蛛网膜下腔出血的发生率较高的原因,但据推测在脑动脉瘤及其破裂的发病机制中存在激素影响。具体地说,绝经后雌激素的丢失在脑动脉瘤的发生中起着一定的作用。一些回顾性研究表明,绝经年龄越早,动脉瘤破裂的风险越高。然而,现有的研究不能解释,多达三分之一的人在动脉瘤破裂时死亡。ASAH的罕见使得获得足够生殖数据的前瞻性研究很难实现。
通过一项名为Nurses' Health Study(NHS)的大型前瞻性队列研究,近日,研究人员调查了女性的生殖寿命、初潮年龄、绝经年龄与口服避孕药或绝经后激素治疗的使用之间的关系。
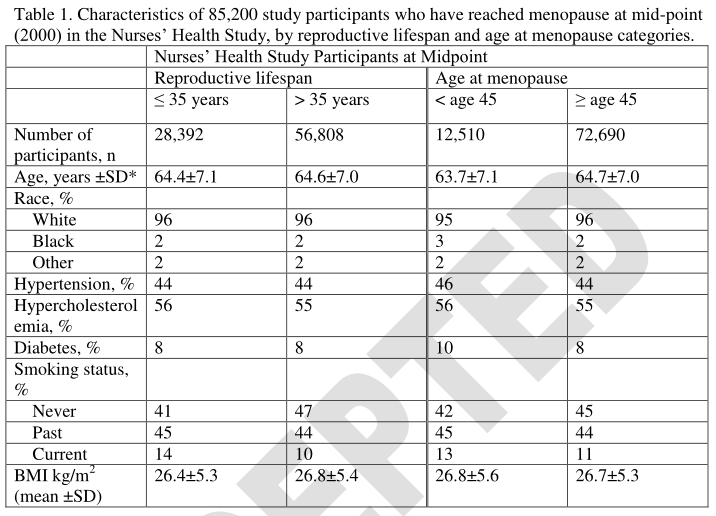
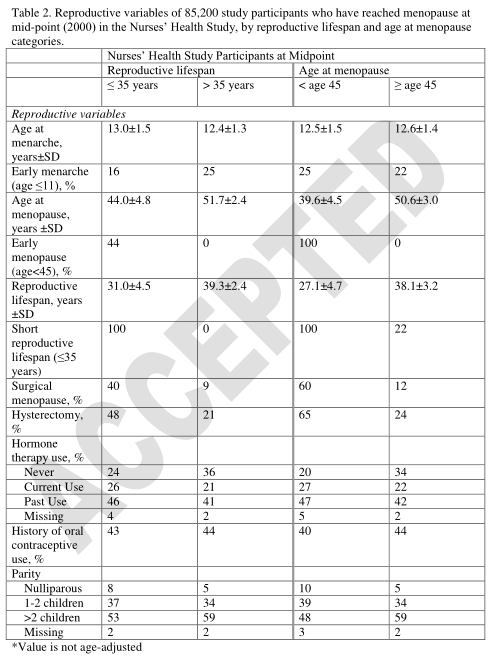
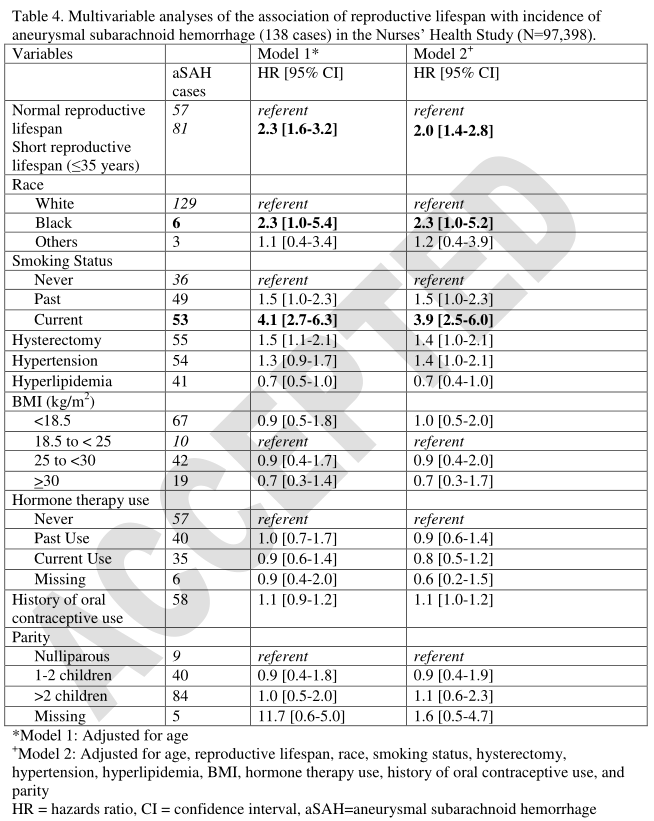
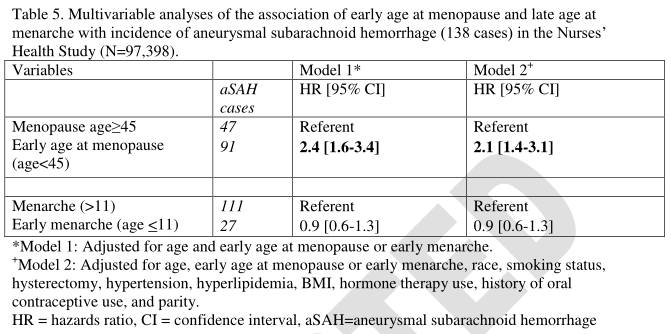
对Nurses' Health Study(NHS)研究的受试者从1980年或绝经后至2018年进行跟踪调查,仅纳入自然绝经或双侧卵巢切除术后绝经的妇女。生殖寿命的定义是从绝经年龄减去月经初潮年龄。采用多变量分层比例风险模型研究生育年限、月经初潮年龄和绝经年龄与ASAH发病率的关系。多变量模型根据年龄、种族、吸烟、子宫切除、高血压、高脂血症、体重指数、激素治疗使用、口服避孕药使用和产次进行了调整。
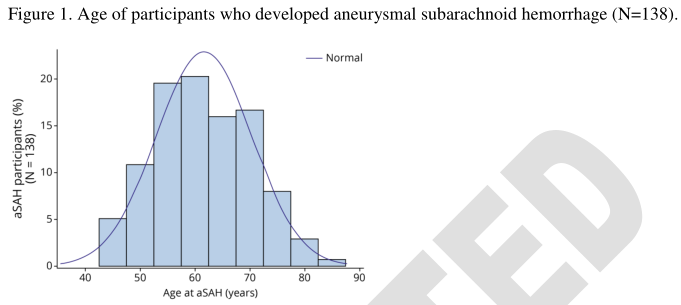
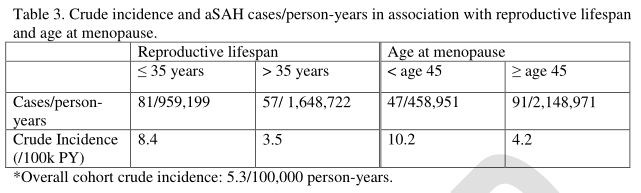
- 共有97,398名有生育寿命数据的绝经后妇女入选,由内科医生检查就诊记录确立,其中138名参与者患上了动脉瘤性蛛网膜下腔出血。
- 经多因素调整后,生育期越短(≤35年),ASAH的发生率增加2倍(HR=2.0[95%CI 1.42.8])。
- 同样,绝经年龄早(45≤岁)与ASAH的风险较高(HR=2.1[95%可信区间1.4-3.1]),但初潮年龄并不相关。
- 口服避孕药的使用和绝经后激素治疗与ASAH的发生率无关。
绝经年龄越早,生殖寿命越短(≤为35岁),女性发生ASAH的风险就越高。没有注意到初潮年龄、产次、口服避孕药使用或绝经后治疗使用的相关性。
文献来源:Rosalind Lai PM, Jimenez M, Du R, Rexrode K. Association of Reproductive Life Span and Age at Menopause With the Risk of Aneurysmal Subarachnoid Hemorrhage [published online ahead of print, 2022 Mar 29]. Neurology. 2022;10.1212/WNL.0000000000200447. doi:10.1212/WNL.0000000000200222
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
38
#aSAH#
40
#ASA#
47
#绝经年龄#
43
#蛛网膜#
40
#绝经#
64
#动脉瘤性蛛网膜下腔出血#
31
#SAH#
33