Nature Neuroscience: 科学家揭示不同脑膜层在大脑自身免疫性疾病的功能差异性
2022-07-07 周科 神经周K
脑膜可分为软脑膜(软脑膜和蛛网膜层)和厚脑膜(硬脑膜层):软脑膜的内层与脑和脊髓的神经组织紧密相连。蛛网膜下腔将蛛网膜层与血管紧密相连的软脑膜分隔开来。
正常生理状态下外周免疫系统几乎无法进入大脑和脊髓实质,但免疫细胞可通过脑膜能够巡逻它们之间的边界:这是脑膜发挥作用的地方。脑膜内密集分布着常驻的免疫活性细胞。此外,T细胞可以在血液、软脑膜和脑脊液之间转运。
脑膜可分为软脑膜(软脑膜和蛛网膜层)和厚脑膜(硬脑膜层):软脑膜的内层与脑和脊髓的神经组织紧密相连。蛛网膜下腔将蛛网膜层与血管紧密相连的软脑膜分隔开来。硬脑膜直接附着在大脑骨结构或通过脊髓硬膜外间隙附着骨结构上。
在疾病状态下(多发性硬化症),这种平衡出现紊乱:脑膜成为致病性免疫T细胞进入大脑实质的主要位点。从免疫学角度来看,硬脑膜可能发挥更积极的作用:拥有自己的血管系统,不存在血-脑或血-脑脊液屏障。
2022年6月30日德国哥廷根大学医学中心Francesca Odoardi课题组发现软脑膜在急性和慢性中枢神经系统自身免疫性疾病中发挥重要作用。

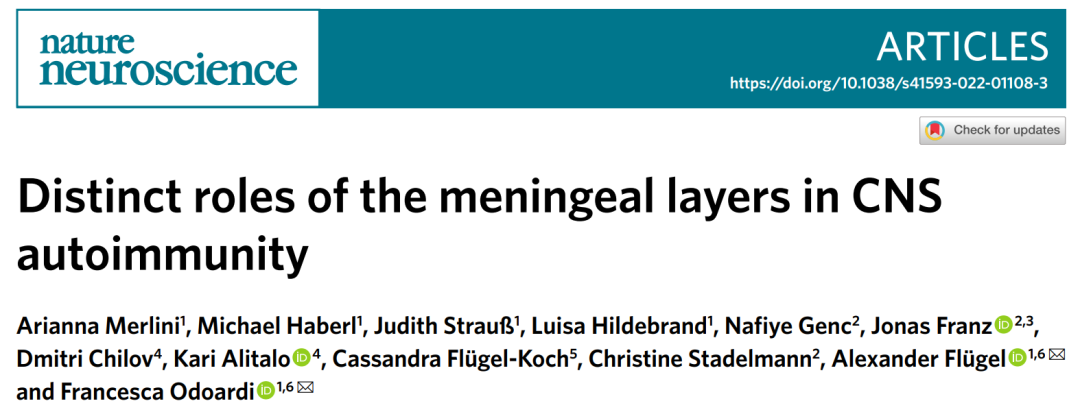
图1:T细胞异常聚集在软脑膜
髓鞘碱性蛋白诱发急性自发性免疫疾病模型中脊髓软脑膜和实质发生强烈炎症:大量T细胞和髓样细胞浸润,但在硬脑膜区域这些致病免疫细胞浸润很少。这种免疫细胞差异性浸润分布的特征也出现在大脑中:整个发病过程中硬脑膜区域免疫细胞浸润数量明显低于软脑膜和实质中。
在多发性硬化症患者中浸润性T细胞出现在软脑膜和硬脑膜中,其中聚集在软脑膜部位的T细胞数量明显比硬脑膜区域多。
静脉注射可通过血脑屏障的荧光示踪剂从血管中渗出,并迅速积聚在硬脑膜的血管周围巨噬细胞中,在软脑膜区域观察不到这种聚集。通过在体显微镜技术发现大量致病T免疫细胞在软脑膜血管内爬行,但在硬脑膜血管中只有极少数细胞这样做。相反,它们松散地沿着内皮细胞移动。这种看似矛盾的结果其实是由于硬脑膜内皮细胞低水平表达紧密连接蛋白引起的。
在反应性脑脊髓炎动物模型中硬脑膜细胞因子和趋化因子水平降低,抗原特异性T细胞的激活也明显降低。更进一步来说硬脑膜来源T细胞表达的促炎症因子水平明显比软脑膜和实质的T细胞更低一些。
硬脑膜T细胞激活减少最终引起T细胞与局部抗原呈递细胞接触能力:T细胞运动速度减慢,在与局部巨噬细胞接触时变得静止不动。
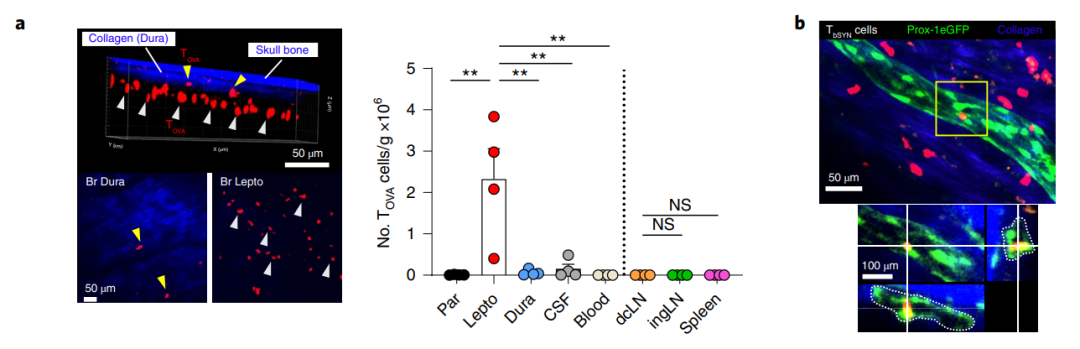
图2:T细胞在软、硬脑膜中的分布
已有研究表明硬脑膜通过硬脑膜淋巴管将中枢神经系统的免疫细胞转运到颈深淋巴结。研究人员向脑脊液中注射卵清白蛋白特异性T细胞后,大多数T细胞聚集在软脑膜,少数细胞聚集在硬脑膜和颈深淋巴结。进一步通过病毒损毁硬脑膜淋巴管后并不影响T细胞浸润到软脑膜中,表明硬脑膜可能并不参与中枢神经系统自身免疫性疾病。
总的来说,本文揭示了不同的脑膜层在中枢神经系统自身免疫性疾病的作用:与软脑膜相比,硬脑膜在急性和慢性自身免疫性疾病中发挥相当“被动”的作用。
原始出处:
Merlini, A., Haberl, M., Strau, J. et al. Distinct roles of the meningeal layers in CNS autoimmunity. Nat Neurosci (2022). https://doi.org/10.1038/s41593-022-01108-3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Nat#
28
学习了
36
#ROS#
43
#SCIE#
37
#免疫性疾病#
0