NEJM:多支血管PCI的完全血运重建治疗心肌梗死效果分析(COMPLETE研究)
2019-10-10 xing.T MedSci原创
由此可见,在STEMI和多支冠状动脉疾病患者中,完全血运重建在减少心血管死亡或心肌梗塞风险以及心血管死亡、心肌梗塞或缺血性血运重建的风险方面优于仅罪犯病变的PCI。
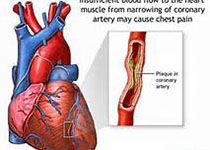
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员将已经成功完成罪犯病变PCI的STEMI和多支冠状动脉疾病患者随机分配对血管造影中非罪犯病变进行PCI的完全血运重建的策略或未进行进一步血运重建。根据非罪犯病变PCI的预期时机(在住院期间或之后)进行随机分组。该研究的第一项主要结局是心血管死亡或心肌梗塞的综合症状;第二项主要结局是心血管死亡、心肌梗塞或缺血性血运重建的综合结局。
中位随访时间为3年,完全血运重建组2016例受试者中有158例患者(7.8%)发生了第一项主要结局,而仅罪犯病变PCI组中2025例患者有213例(10.5%)发生了第一项主要结局(风险比为0.74; 95%置信区间[CI]为0.60至0.91;P=0.004)。完全血运重建组中有179例患者(8.9%)发生了第二项主要结局,而仅罪犯病变PCI组中有339例患者(16.7%)(风险比为0.51;95%CI为0.43至0.61);P<0.001)。对于这两种主要的结局,无论非病灶性PCI的预期时机如何,始终可观察到完全血运重建的益处(对于第一项和第二项主要结局的相互作用P=0.62和P=0.27)。
由此可见,在STEMI和多支冠状动脉疾病患者中,完全血运重建在减少心血管死亡或心肌梗塞风险以及心血管死亡、心肌梗塞或缺血性血运重建的风险方面优于仅罪犯病变的PCI。
原始出处:
Shamir R. Mehta,et al.Complete Revascularization with Multivessel PCI for Myocardial Infarction.NEJM.2019.https://www.nejm.org/doi/full/10.1056/NEJMoa1907775
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#效果分析#
36
#完全血运重建#
35
#多支血管#
37
#多支血管PCI#
25
#complete#
26
#MPL#
24
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
40
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
40