Laryngoscope:步态和年龄相关的听力损失对整体认知和跌倒的影响
2021-10-28 AlexYang MedSci原创
调查了步态和ARHL对老年人整体认知和跌倒的影响。
年龄相关听力损失(ARHL)是老年人的一个常见问题,可导致沟通困难。ARHL也会引起其他健康问题,特别是认知障碍和跌倒。既往一项大型队列研究显示,ARHL与认知能力下降速度的增加和患痴呆症风险的增加有关,并且这两种情况发生的可能性随着ARHL严重度的增加而增加。此外,跌倒在ARHL老年人中很普遍;最近的一项荟萃分析报告指出,ARHL老年人跌倒的几率是听力正常者的2.39倍。
年龄相关的听力损失(ARHL)是认知障碍和跌倒的一个风险因素,且该关联可能受步态的调节。近期,来自日本的研究人员调查了步态和ARHL对老年人整体认知和跌倒的影响。
在1000和4000Hz下,研究人员测量了810名社区老年人的纯音平均听觉阈值,获得听觉敏锐度数据。然后将参与者分层如下:正常听力,≤25分贝;轻度听力损失(HL),>25和≤40分贝;中度至重度HL,>40分贝。研究人员使用计时器测量了他们的步态速度,并作为步态表现和跌倒发生率的一个指标。跌倒发生率由参与者回想获得,并记录了相关的社会人口和临床变量,包括年龄、性别、用药等情况。还使用了蒙特利尔认知评估(MoCA)测试确定整体认知能力。IBM SPSS和多元逻辑回归用来分析相关数据。
结果表明,共有320名(39.5%)和233名(28.8%)参与者分别患有轻度和中度至重度HL。多元逻辑回归分析显示,在整体认知和跌倒的发生中,步态表现与中度听力损失均存在相互作用。具体来说,患有中度听力损失的老年人如果行走缓慢,其MoCA得分较低,跌倒的发生率较高,而那些步态速度较快的老年人则没有表现出这种倾向。
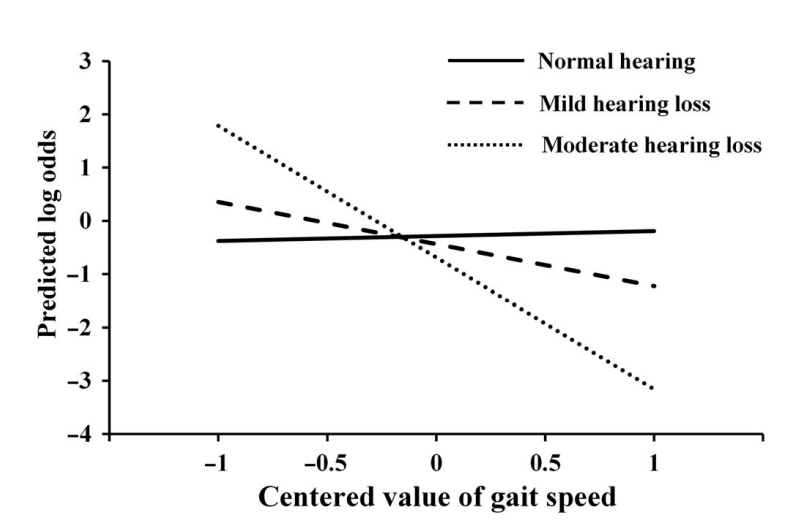
听力损失与步态速度的相互作用对跌落的影响
综上所述,不良的步态表现可能会改变ARHL的影响,并导致认知能力下降和跌倒。另外,认知能力差和跌倒可能在患有ARHL的老年人中普遍存在,尤其是步态较慢和患有中度听力损失的人。
原始出处:
Ryota Sakurai , Hisashi Kawai , Shuichi Yanai et al. Gait and Age-Related Hearing Loss Interactions on Global Cognition and Falls. Laryngoscope. Oct 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#步态#
36
#年龄相关#
33
#PE#
39
#听力#
45