Leukemia :罗特西普用于骨髓增生异常综合征/骨髓增生性肿瘤伴环状铁粒幼细胞和血小板增多症
2022-03-03 MedSci原创 MedSci原创
骨髓增生异常综合征/骨髓增生性肿瘤伴环状铁粒幼细胞和血小板增多症 (MDS/MPN-RS-T) 是一种具有骨髓增生异常和骨髓增生特征的骨髓疾病。MDS/MPN-RS-T相关性贫血会导致疲劳、生活质量下

骨髓增生异常综合征/骨髓增生性肿瘤伴环状铁粒幼细胞和血小板增多症 (MDS/MPN-RS-T) 是一种具有骨髓增生异常和骨髓增生特征的骨髓疾病。MDS/MPN-RS-T相关性贫血会导致疲劳、生活质量下降和生存恶化,其治疗旨在改善贫血、降低血栓事件风险、降低血小板和/或改变病程。然而,支持这些治疗效果的数据很少。
罗特西普是一流的红细胞成熟剂,可结合多种转化生长因子-β 超家族配体,增强晚期红细胞生成。一项3 期 MEDALIST 研究 (NCT02631070)的结果使其获得美国食品和药物管理局和欧洲药品管理局的批准,用于治疗患有低风险 MDS-RS 或 MDS/MPN-RS 的成人贫血-T 在红细胞生成刺激剂 (ESA) 失败后需要 ≥2 RBC 单位/8 周。此处报告了 MEDALIST 研究中对 MDS/MPN-RS-T 患者的罗特西普疗效和安全性的事后分析。
MEDALIST 研究招募了 229 名患有低风险 MDS-RS 的成年人,他们需要 ≥2 RBC 单位/8 周,并且对 ESA 不耐受或不耐受。患者按 2:1 随机分配至罗特西普或安慰剂组,每 3 周皮下给药,持续 24 周。罗特西普起始剂量为 1.0 mg/kg,根据输血要求和不良事件滴定至最大 1.75 mg/kg。使用细胞形态学、细胞遗传学和分子遗传学结果以及血细胞计数对意向治疗人群中的 MDS/MPN-RS-T 患者进行诊断。
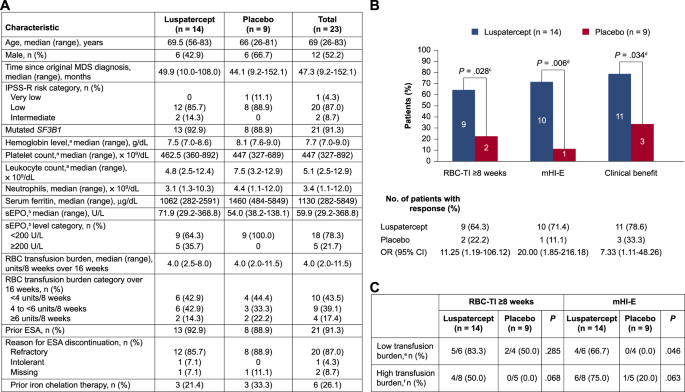
在 MEDALIST 研究的 229 名患者中,23 名 (10.0%) 患有 MDS/MPN-RS-T;14 人被随机分配到罗特西普组,9 人被随机分配到安慰剂组。两组之间不同的基线特征包括较低的中位白细胞计数(4.8 vs 7.5 × 10 9 /dL)和血清铁蛋白(1062 vs 1460 µg/dL),以及较高的血清促红细胞生成素(sEPO)(71.9 vs 54.0 U/L) (图 1A)。罗特西普和安慰剂组的中位(范围)随访时间分别为 27.4(3.5-35.6)和 13.8(3.3-32.2)个月。
图 1:MEDALIST 试验中 MDS/MPN-RS-T 患者的基线特征和治疗反应。
MEDALIST 研究的主要终点是第 1-24 周期间 RBC 输血独立性 (RBC-TI) ≥8 周。次要终点包括:改良的血液学反应——红细胞(mHI-E;平均血红蛋白增加 ≥1.5 g/dL [基线时接受 <4 RBC 单位/8 周的患者]或减少 ≥4 单位 RBC 输血[接受 ≥4 RBC 的患者单位/基线 8 周],连续 56 天以上);在第 1-24 周内连续 56 天从基线增加≥1.0 g/dL 血红蛋白;进展为急性髓性白血病(AML) 的速度;和治疗中出现的不良事件 (TEAE) 的发生率。还进行了临床益处的事后分析(定义为 RBC-TI ≥8 周和/或第 1-24 周期间的 mHI-E)。所有P值都是描述性的,未针对多重性进行调整。
截至 2019 年 7 月,随机分配到罗特西普的MDS/MPN-RS-T 患者在第 1-24 周期间达到 RBC-TI ≥8 周的比例显着增加(64.3 对 22.2%;P = 0.028);mHI-E(71.4 对 11.1%;P = 0.006);和临床获益(78.6 对 33.3%;P = 0.034),与安慰剂相比(图 1B)。罗特西普组从临床获益开始到治疗结束的中位时间为 94.6周,安慰剂组为 23.9(范围 23.7-57.9)周。
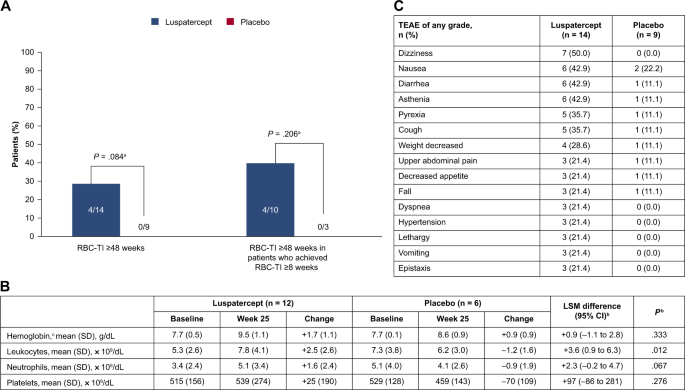
随机分配到罗特西普组与安慰剂组的低输血负担患者(<4 个单位/8 周)的数值更高,RBC-TI ≥8 周(5/6 [83.3%] vs 2/4 [50.0%];P = 0.285)在第 1-24 周内,实现 mHI-E 的比例显着增加(4/6 [66.7%] vs 0/4 [0.0%];P = 0.046)(图 1C)。随机分配到罗特西普组与安慰剂组的高输血负担患者(≥4 个单位/8 周)的数值更高,RBC-TI ≥8 周(4/8 [50.0%] vs 0/5 [0.0%];P = 0.068)和 mHI-E(6/8 [75.0%] vs 1/5 [20.0%];P = 0.063)(图 1C)。64.3% 的患者随机分配到罗特西普组,而安慰剂组为 33.3%,第 1-48 周 RBC-TI ≥8 周(P = 0.088)。随机分配至罗特西普组的患者与无安慰剂组的患者相比,28.6% 的患者在治疗期间的任何时间都达到了 RBC-TI ≥48 周;在治疗期间任何时间 RBC-TI ≥ 8 周的罗特西普组患者中,40.0% 的患者 RBC-TI ≥ 48 周,而没有安慰剂患者(图 2A)。
图 2:治疗反应、实验室参数和 TEAE
尽管数量有限,但通过与整个 MEDALIST 研究人群的数据进行比较,支持了罗特西普对 MDS/MPN-RS-T 患者的价值。MDS/MPN-RS-T 患者在第 1-24 周内 RBC-TI ≥8 周的实现率(64.3 对 22.2%)高于 MEDALIST 总体人群(37.9 对 13.2%)。同样,随机分配到罗特西普和安慰剂组的 MDS/MPN-RS-T 患者中有 71.4% 对 11.1% 的患者实现了 mHI-E,而 MEDALIST 总体人群中的这一比例为 52.9% 对 11.8%。
治疗 24 周后,随机分配至罗特西普的患者的平均血红蛋白、白细胞和中性粒细胞较基线升高,而血小板水平保持稳定(图 2B)。虽然 24 周后 MDS/MPN-RS-T 患者的血红蛋白水平升高在罗特西普和安慰剂之间没有显着差异,但绝对升高幅度名义上更高。随机分配到罗特西普与安慰剂组的患者平均白细胞计数显着增加,但平均血小板或中性粒细胞计数没有增加。在基线时,MDS/MPN-RS-T 患者的血小板计数中位数高于 MEDALIST 总体人群,正如预期的那样,sEPO 中位数较低,接受铁螯合治疗的可能性较小,输血负担中位数较低,这与他们较高的 RBC-TI 和 mHI-E 反应率一致。
罗特西普组最常见的任何级别的 TEAE 是头晕、恶心、腹泻和虚弱(图2B)。导致停药的 TEAE 发生在罗特西普组 14 名患者中的 2 名(14.3%)和安慰剂组9名患者中的3名(33.3%)。一名随机分配到罗特西普的患者经历了短暂性脑缺血发作。一名随机分配到安慰剂组的患者进展为 AML(P = 0.202),而没有随机分配到罗特西普组。
对 MDS/MPN-RS-T 患者的治疗建议包括 ESA 和贫血输血,来那度胺治疗贫血和血小板水平降低 。对 MDS/MPN-RS-T 患者使用来那度胺的建议基于 12 例患者的病例报告和167例患者的回顾性分析,而不是临床试验;ESA 的使用基于一项单一的回顾性研究,该研究包括 40 名 MDS/MPN-RS-T 患者,其中 45% 达到红系反应(血红蛋白增加≥2.0 g/dL 或 RBC-TI ≥8 周的患者)要求 ≥4 个单位/8 周),而目前研究中接受罗特西普(难治性或不适合 ESAs)治疗的患者占 71.4%。然而,鉴于红系反应的不同定义,这种比较应谨慎进行。
总之,该亚组分析提供了第一个临床试验数据,以支持罗特西普对MDS/MPN-RS-T患者的疗效。总体而言,罗特西普被发现是有效的——显着降低输血负担并改善 mHI-E 和白细胞水平——具有普遍良好耐受的安全性。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#增生性#
68
#骨髓增生异常综合#
61
#血小板增多症#
53
#骨髓增生异常#
46
#骨髓增生#
62
学习了很多学习了学习了
78
期待
97
学习学习学习学习危重症学习学习学习学习学习学习学习学习学习学习
93
感谢分享
96
学习了,谢谢分享
83