Circulation-Cardiovascular Interventions:冠脉内应用肾上腺素和腺苷对血压正常的急性冠脉综合征患者无复流情况影响的比较(COAR试验)
2022-01-19 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
急诊PCI是目前急性冠脉综合征(ACS)的首选治疗手段,能在短时间内有效开通大血管,从而挽救患者生命。然而大血管再通并不意味着心肌组织在微循环水平恢复再灌注,也不一定意味着缺血心肌细胞都可以被挽救活。
急诊PCI是目前急性冠脉综合征(ACS)的首选治疗手段,能在短时间内有效开通大血管,从而挽救患者生命。然而大血管再通并不意味着心肌组织在微循环水平恢复再灌注,也不一定意味着缺血心肌细胞都可以被挽救存活,其中心肌无复流是主要原因之一。2022年1月10日,一项发表于Circulation:Cardiovascular Interventions的开放标签、随机对照研究表明,对于血压正常的ACS患者而言,冠脉内应用肾上腺素比肝素能更安全、有效地改善PCI术后无复流情况。
研究目的
无复流是指心外膜冠脉闭塞经急诊介入治疗已得到正常开通,但由于微循环水平血流仍不能完全恢复,使缺血心肌组织无有效再灌注的现象,表现为冠脉血流减慢(TIMI血流≤2级,未达正常的TIMI 3级)或无复流(TIMI血流0级或1级)。这一现象在急性冠脉综合征患者中发生率高达32%,尤其是在冠状动脉旁路移植术(CABG)后静脉桥血管(SVG)病变的介入手术和冠脉旋磨术中。
无复流出现预示着不良预后,常导致左心室功能障碍、进展性的心肌损害以及病死率增加,因此早期识别无复流的高危患者并积极实施相关干预措施非常重要。冠脉内给药是目前临床中最常见的无复流干预策略之一。常用药物(包括腺苷、维拉帕米、硝普钠和尼卡地平)均能有效改善患者冠脉血流情况并获得更好的预后情况;然而,冠脉无复流的患者往往表现出血压降低的临床症状,不适用与上述常用药物。在这种情况下,肾上腺素或成为临床医师的唯一选择。
由于肾上腺素应用于PCI术后无复流患者的相关研究数据较少,因此该研究旨在探索肾上腺素是否可以作为无法应用腺苷恢复冠脉内血流动力学或效果有限患者(尤其是出现低血压和心动过缓症状时)的一线或替代药物。
研究方法
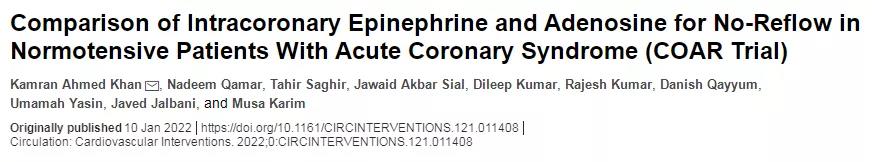
本研究是一项开放性标签的随机对照试验,共纳入201例在2020年12月至2021年5月期间于美国国家心血管疾病研究所住院的ACS患者。所有纳入患者的年龄≥18岁,基线收缩压≥100 mmHg,且出现无复流症状(即在PCI术后TIMI血流分级≤2级)。排除标准包括:基线收缩压≤100 mmHg、瓣膜病或先天性心脏病、对肾上腺素或腺苷过敏、阿司匹林或氯吡格雷禁忌证、心肌病、心包炎、心肌炎。(图1)
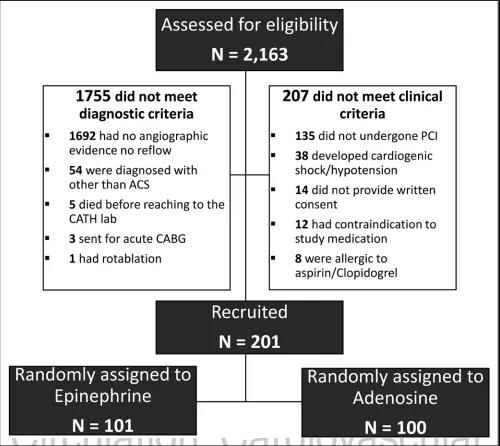
图1. 研究患者纳入流程图
所有纳入患者按照1:1的比例随机分配至肾上腺素组(101例)和腺苷组(100例),分别采取100-600 μg肾上腺素/60-1000 μg腺苷联合或不联合100-1000 μg硝普钠,药物最终的用量取决于是否达到主要终点或血流动力学稳定。同时,所有患者被给予300 mg口服阿司匹林、氯吡格雷以及静脉注射70-100 U/kg肝素以维持250-300 s的ACT时间,并按照ACC/AHA指南给予IIa/IIIb受体拮抗剂。
该研究的主要结果为冠脉内给药后依据校正的TIMI帧数(cTFC)和心肌呈色分级(MBG)评价达到TIMI血流3级;次要结果为全因死亡率和主要不良心血管事件发生率,包括心律失常、复发MI、重复血运重建、脑血管事件和心力衰竭。
研究结果
肾上腺素组和腺苷组的硝普钠应用比例为75.2% vs. 88%(P=0.020),IIa/IIIb受体拮抗剂应用比例为23.8% vs. 20%(P=0.519);肾上腺素、腺苷的平均应用剂量分别为318.42±255.97 μg、269.5±167.79 μg;两组的硝普钠平均应用剂量分别为318.42±255.97和380.68±275.3(P=0.098)。在肾上腺素组中,有5.96%患者出现显着但可耐受的≤160 b/min的自限性心率升高,3.94%患者出现≥200 mmHg的自限性收缩压升高;其外,有≤2%的患者出现室性心动过速,其中1例患者自行恢复窦性心律,2例患者需要行直流电复律;1.9%患者出现恶心或呕吐。在腺苷组中,7%患者出现恶心或呕吐,7%患者出现自限性窦性心动过缓。
肾上腺素组和腺苷组中患者血流恢复TIMI 3级的比例分别为90.1% vs. 78%(P=0.019);两组的最终cTFC值分别为24±8.43 vs. 26.63±9.22(P=0.036),但平均cTFC减少值分别为-25.71±11.79 vs. -26.08±11.71(P=0.825)(图2);两组达到MBG 3级的概率分别为55.4% vs. 45%(P=0.134)(图3)。而两组的次要结果终点无明显统计学差异。值得注意的是,肾上腺素组中术后评估显示LVEF值≥40%的患者明显多于腺苷组(40.9% vs. 22.9%)。

图2. PCI术中应用冠脉内给药前后两组的cTFC值对比
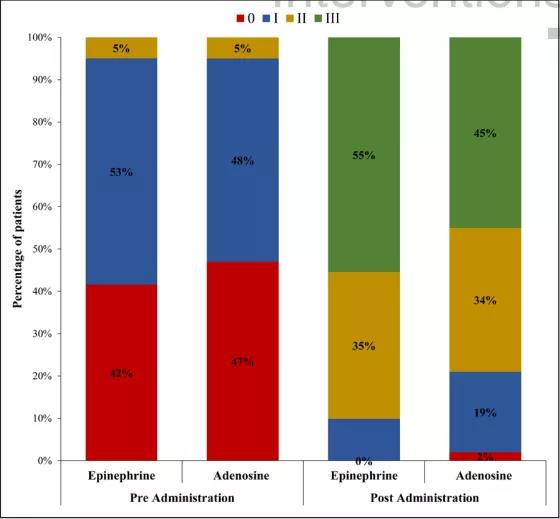
图3. PCI术中应用冠脉内给药前后两组的MBG分级对比
总结
肾上腺素对于治疗出现无复流的血压正常的ACS患者而言是相对安全的。相较于腺苷,术中行肾上腺素的冠脉内给药后可显着提升TIMI血流分级、降低cTFC值,且MBG分级亦有较为理想的改善;但其在由全因死亡率和主要心脏不良事件影响的住院率和短期临床获益方面与腺苷较为类似。
讨论
在该研究招募的ACS患者群体中,当PCI术中出现STEMI时出现无复流症状的可能性最高,冠脉内旋磨术和静脉桥血管病变介入次之。由于静脉桥血管病变的患者临床症状较为少见或未满足标准、冠脉内旋磨术患者非ACS情况,这两类患者在最终未纳入试验。
目前,TIMI血流分级是临床中最常见的冠脉血流水平分级手段,尽管其分级标准被不断完善但无法彻底消除不同术者之间对血流判断上的差异。为了解决这一问题,本研究引入cTFC和MBG以更全面、直接地反应冠状动脉微血管功能,从而有助于术者判断是否出现无复流。
本研究结果显示,肾上腺素给药的耐受性较为良好,除了小部分患者出现可控的不良反应,而腺苷组的硝普钠应用率较肾上腺素更高(88% vs. 75.2%,P=0.020);此外,肾上腺素组的冠脉内血流恢复情况更优、cTFC值更低、MBG 3级的比例和术后LVEF值更高,这说明相较于腺苷,肾上腺素的安全性和有效性更佳。然而,值得注意的是,两组的IIa/IIIb受体拮抗剂应用率、30天全因死亡率和主要心血管事件发生率方面无明显统计学差。
尽管肾上腺素在过去的研究中已经被证实可用于难治性ACS患者的无复流,但对其在正常血压患者中的临床获益是有一定争议的。作为目前为止对比肾上腺素和腺苷临床获益的最大规模的临床试验,本研究为肾上腺素成为出现该类患者的一线药物提供了强有力的证据。但本试验仍存在一定局限性,如单中心招募等,可能存在一定的选择偏移,因此仍需更大的多中心试验以进一步说明。
原始出处:
Kamran Ahmed Khan, Nadeem Qamar, Tahir Saghir, et al. Comparison of Intracoronary Epinephrine and Adenosine for No-Reflow in Normotensive Patients With Acute Coronary Syndrome (COAR Trial). Circulation: Cardiovascular Interventions. 2022;0:CIRCINTERVENTIONS.121.011408.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASC#
54
#COA#
52
#肾上腺#
44
#vascular#
46
#血压正常#
57
这是值得学习的
49
#肾上腺素#
67
#综合征#
34
#cardiovascular#
51