JAHA:高敏肌钙蛋白T和I浓度与CAD患者全因死亡率和心血管结局的关联
2022-07-20 MedSci原创 MedSci原创
在调整典型心血管危险因素、低密度脂蛋白胆固醇、估计的肾小球滤过率、hs-CRP、NT-proBNP和CAD严重程度后,hsTnT和hsTnI与全因死亡率独立相关。
高敏感性肌钙蛋白T(hsTnT)和高敏感性肌钙蛋白I(hsTnI)与冠状动脉疾病(CAD)患者结局之间的相关性在很大程度上仍是未知的。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是探讨hsTnT和hsTnI血液水平是否会随着CAD严重程度的增加而增加,并为稳定CAD患者未来主要不良心血管事件和全因死亡率提供额外的预测信息。
接受冠状动脉造影和hsTnT和hsTnI检查的Interath队列患者被纳入研究。研究人员通过hsTnT(RocheElecsys)和hsTnI(AbbottARCHITECTSTAT)定量肌钙蛋白浓度。为了研究hsTnT和hsTnI与预后之间的关系,研究人员进行了一项多变量分析,并调整了典型心血管危险因素、低密度脂蛋白胆固醇、估计的肾小球滤过率、hs‐CRP(高敏感性C‐反应蛋白)、NT‐proBNP(脑钠肽前体N‐端)和Gensini评分。
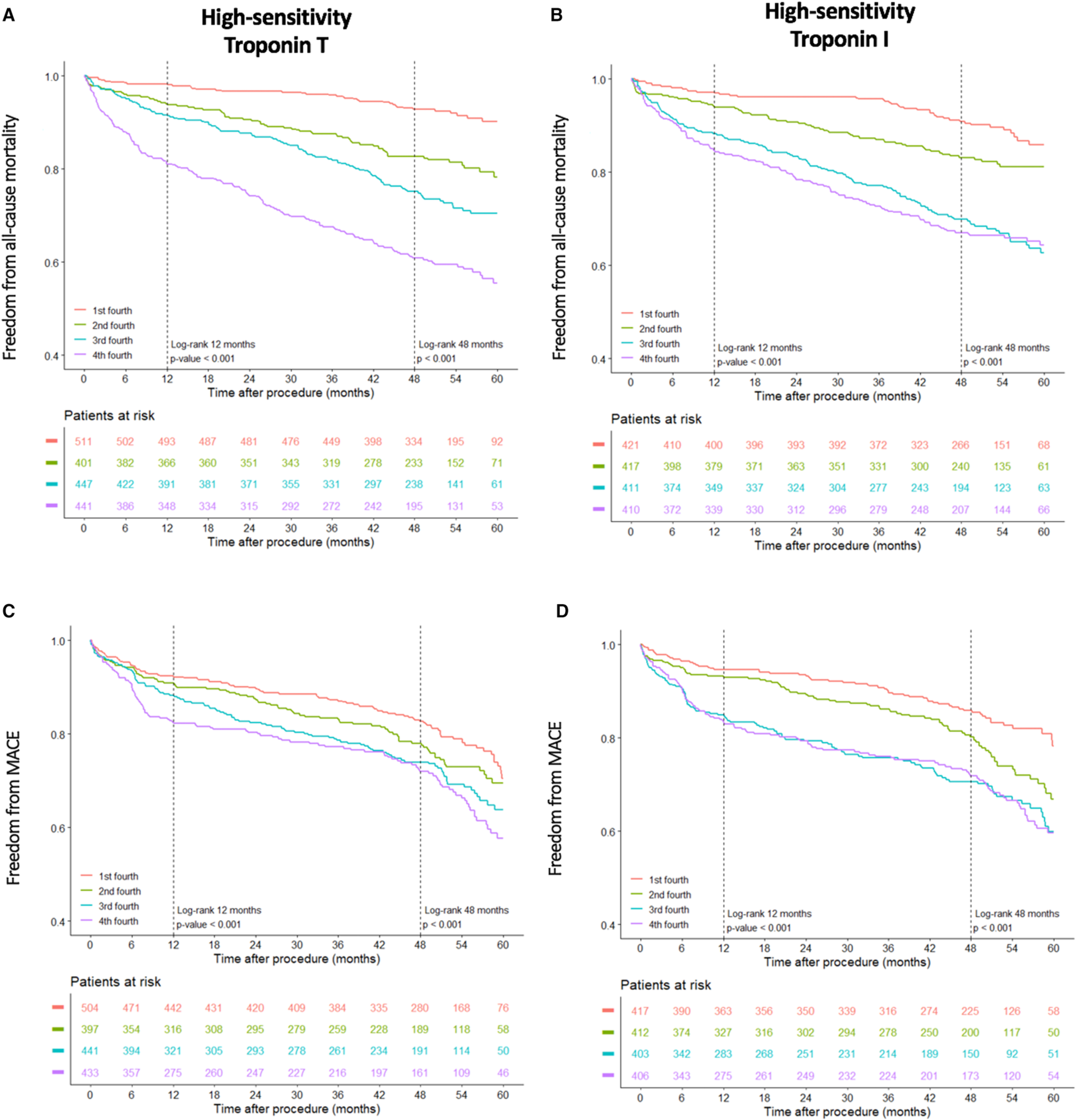
1829例患者中27.9%为女性,平均年龄为68.6±10.9岁。确诊为CAD的患者的肌钙蛋白血浓度高于未确诊的患者。使用线性回归模型,当前吸烟、动脉高血压、估计的肾小球滤过率、hs-CRP、NT-proBNP以及根据Gensini和SYNTAX评分分级的CAD严重程度与高敏感性肌钙蛋白水平相关。患者随访4.4年(第25和75百分位:4.3-4.4)。经多变量调整后,hsTnT(风险比[HR]为1.7[95%CI为1.5-2.2],P<0.001)和hsTnI(风险比为1.5[95%CI为1.2-1.8],P<0.001)预测了全因死亡率。然而,在校正了包括冠心病严重程度在内的大多数可能混杂因素后,只有hsTnI(HR为1.2[95%CI为1.0-1.4],P=0.032)仍然是主要不良心血管事件的独立预测因子(hsTnT:HR为1.0[95%CI为0.9-1.2],P=0.95)。
由此可见,在调整典型心血管危险因素、低密度脂蛋白胆固醇、估计的肾小球滤过率、hs-CRP、NT-proBNP和CAD严重程度后,hsTnT和hsTnI与全因死亡率独立相关,但在接受冠状动脉造影的稳定患者中,只有hsTnI与主要不良心血管事件相关。
原始出处:
Benjamin Bay.et al.Association of High‐Sensitivity Troponin T and I Blood Concentrations With All‐Cause Mortality and Cardiovascular Outcome in Stable Patients—Results From the INTERCATH Cohort.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.024516
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#全因死亡率#
58
#AHA#
36
#心血管结局#
66
#浓度#
52
#肌钙蛋白T#
50