新研究评估Masimo SedLine®脑功能监护仪能否预测心跳骤停后ICU患者的神经系统转归和长期生存
2021-07-07 国际文传 网络
研究人员发现,患者状态指数(PSi)和抑制率(SR)这两个SedLine参数联用,可以非常准确地预测心跳骤停后180天的死亡率
瑞士纳沙泰尔--(美国商业资讯)--Masimo (NASDAQ: MASI)今天宣布在《危重医学杂志》(Journal of Critical Care)上发表的一项研究结果,该研究中,韩国东国大学医学院和延世大学医学院的Tae Youn Kim博士及其同事评估了Masimo SedLine®脑功能监护仪提供的两个参数能否预测心跳骤停后ICU患者的神经系统转归和长期生存1。研究人员发现,患者状态指数(PSi)和抑制率(SR)这两个参数联用可“非常准确地预测”心跳骤停后180天的死亡率。
研究人员指出,心跳骤停后患者的“精准预后”对于确定治疗计划和“继续或撤离重症监护室与否”至关重要,并且人们建议采用“多管齐下”的方法,因为“尚无单一的预后因素被证明预后精度高于其他因素”,因此寻求评估两个Masimo SedLine参数单用或联用时预测神经系统转归的预后精度。研究人员选用PSi是因为,正如他们所指出的,原始EEG数据可能“难以使用”,而源自EEG的PSi广泛用于麻醉以确定手术镇静的程度,在全身麻醉下“与状态变化显著协变”,并“能显著预测”麻醉剂施药不同阶段的觉醒水平。研究人员选择SR是因为它有助于估计EEG抑制的百分比,因此被认为是神经系统转归不良的良好预测指标2。
他们在2017年1月至2020年8月间募集103例成人患者,这些患者经历了非创伤性院外心跳骤停,在CPR后成功复苏,并在ICU住院期间接受有针对性的体温管理。从入住ICU后当即到自主循环恢复(ROSC)后24小时,使用Masimo SedLine连续监测PSi和SR,每一小时记录一次。使用匹兹堡脑干评分(PBSS)和脑功能分类(CPC)对神经系统转归进行分类。通过电话访谈获取180天时的生存数据。
研究人员发现,单用PSi或SR可“准确预测”神经系统转归不良,而低PSi和SR联用可“非常准确地预测”心跳骤停后180天的死亡率。他们使用受试者工作特征(ROC)曲线来确定“平均PSI ≤ 14.53和平均SR > 36.6显示高诊断准确性”作为他们研究中患者的单一预后因素。此外,“使用平均PSi和平均SR的多模态预测显示曲线下面积最高值为0.965(95%置信区间为0.909–0.991)。”该研究队列中,平均PSi ≤ 14.53且平均SR > 36.6的患者(该组死亡率为69%)“长期死亡率相对高”于平均PSi > 14.53且平均SR ≤ 36.6的患者(该组死亡率为11%)。
研究人员的结论是:“PSi和SR是心跳骤停后患者早期神经预后的良好预测指标。”他们同时指出:“与各参数单用相比,PSI和SR联用可更准确预测神经系统转归不良。”
关于Masimo
Masimo (NASDAQ: MASI)是一家全球性医疗技术公司,开发生产品种广泛的业界领先的监护技术,包括创新测量设备、传感器、患者监护仪、自动化及互通解决方案。我们的使命是改善患者转归、降低治疗成本,并将无创监护送达新的场景和应用。1995年,公司推出了Masimo SET®移动和低灌注下测量(Measure-through Motion and Low Perfusion™)脉搏氧饱和度仪,100多项独立客观研究显示其性能优于其他脉搏氧饱和度仪技术3。研究显示,Masimo SET®可帮助临床医生减少早产新生儿的重度视网膜病变4、改善新生儿的CCHD筛查5,在用于术后病房的Masimo Patient SafetyNet™连续监测时,可减少快速响应团队动员、ICU转运和成本6-9。Masimo SET®据估计已应用于全世界领先医院及其他医疗机构中超过2亿的患者10,是《美国新闻与世界报道》2020-21年至优医院荣誉榜排名前10位医院中9家医院采用的主要脉搏氧饱和度仪11。Masimo不断优化SET®,2018年宣布,移动状态下RD SET®传感器上的SpO2精度获得显著提高,使临床工作者更加确信,他们所仰赖的SpO2值精确反映了患者的生理状态。2005年,Masimo推出了rainbow®脉搏碳氧-氧饱和度仪技术,实现了以往只能侵入性测量的血液成份的无创连续监测,包括总血红蛋白(SpHb®)、氧含量(SpOC™)、碳氧血红蛋白(SpCO®)、高铁血红蛋白(SpMet®)、脉搏灌注变异指数(PVi®)、RPVi™ (rainbow® PVi)、氧储备指数(ORi™)。2013年,Masimo推出了Root®患者监测和互通平台,该平台从头开始设计,尽可能灵活和具有可扩展性,以便添加其他Masimo和第三方监护技术。关键的Masimo添加包括下一代SedLine®脑功能监护仪、O3®局部氧饱和度仪、搭配NomoLine®取样线缆的ISA™二氧化碳分析仪。Masimo的连续及点检监护仪脉搏碳氧-氧饱和度仪®家族包括旨在用于各类临床及非临床场合的设备,包括无线可穿戴技术(例如Radius-7®和Radius PPG™)、便携式设备(例如Rad-67®)、指尖脉搏氧饱和度仪(例如MightySat®Rx)、医院及居家两用设备(例如Rad-97®)。Masimo院内自动化和互通解决方案以Masimo Hospital Automation™平台为中心,包括Iris® Gateway、iSirona™、Patient SafetyNet、Replica™、Halo ION™、UniView®、UniView:60™、Masimo SafetyNet™。欲了解Masimo及其产品的进一步信息,请访问www.masimo.com。有关Masimo产品的已发表临床研究,请访问www.masimo.com/evidence/featured-studies/feature/。
ORi和RPVi未获得FDA 510(k)认证,未在美国上市。Patient SafetyNet商标由University HealthSystem Consortium授权使用。
参考文献
- Kim TY, Hwang SO, Jung WJ, et al. Early neuroprognostication with the Patient State Index and suppression ratio in post-cardiac arrest patients. J Crit Care. 2018. https://doi.org/10.1016/j.jcrc.2020.06.003(Kim TY、Hwang SO、Jung WJ等。心跳骤停后患者中患者状态指数和抑制率的早期神经预后意义。《危重医学杂志》2018. https://doi.org/10.1016/j.jcrc.2020.06.003)
- Seder DB, Fraser GL, Robbins T, Libby L, Riker RR. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensive Care Med 2010;36(2):281-8.(Seder DB、Fraser GL、Robbins T、Libby L、Riker RR。双谱指数和抑制率是心跳骤停后治疗性低温期间神经系统转归的极早期预测指标。《重症监护医学》2010;36(2):281-8.)
- 有关已发表的脉搏氧饱和度临床试验和Masimo SET®优势的信息,请访问该公司的网站http://www.masimo.com。对照研究包括一些独立、客观的研究,后者包括科学会议上呈报的摘要和同行评议期刊上的论著。
- Castillo A et al. Prevention of Retinopathy of Prematurity in Preterm Infants through Changes in Clinical Practice and SpO2 Technology. Acta Paediatr. 2011 Feb;100(2):188-92.(Castillo A等。通过临床实践转变和SpO2技术预防早产儿视网膜病变。《儿科学报》2011年2月;100(2):188-92.)
- de-Wahl Granelli A et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39,821 newborns. BMJ. 2009;Jan 8;338.(de-Wahl Granelli A等。脉搏氧饱和度筛查对导管依赖型先天性心脏病检出的影响:瑞典39,821例新生儿前瞻性筛查研究。《英国医学杂志》2009年1月8日;338.)
- Taenzer A et al. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010:112(2):282-287.(Taenzer A等。脉搏氧饱和度监测对救治事件和重症监护室转床的影响:前后巧合研究。《麻醉学》2010; 112(2):282-287.)
- Taenzer A et al. Postoperative Monitoring – The Dartmouth Experience. Anesthesia Patient Safety Foundation Newsletter. Spring-Summer 2012.(Taenzer A等。术后监护——达特茅斯经验。《麻醉患者安全基金会通讯》2012年春夏刊。)
- McGrath S et al. Surveillance Monitoring Management for General Care Units: Strategy, Design, and Implementation. The Joint Commission Journal on Quality and Patient Safety. 2016 Jul;42(7):293-302.(McGrath S等。普通监护病房的监测监护管理:策略、设计和执行。《质量与患者安全联合委员会杂志》2016年7月;42(7):293-302.)
- McGrath S et al. Inpatient Respiratory Arrest Associated With Sedative and Analgesic Medications: Impact of Continuous Monitoring on Patient Mortality and Severe Morbidity. J Patient Saf. 2020 14 Mar. DOI: 10.1097/PTS.0000000000000696.(McGrath S等。镇静剂和镇痛剂相关的住院患者呼吸骤停:连续监测对患者死亡率和重度病损率的影响。《患者安全杂志》2020年3月14日。DOI: 10.1097/PTS.0000000000000696.)
- 估计值:Masimo存档数据。
- http://health.usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview。
前瞻性陈述
本新闻稿包含美国《1933年证券法案》第27A条和《1934年证券交易法案》第21E条以及《1995年私人证券诉讼改革法案》所定义的前瞻性陈述。这些前瞻性陈述包含有关Masimo SedLine®潜在功效的各类陈述,等等。这些前瞻性陈述基于对影响我们的未来事件的当前预期,并受到风险和不确定性的制约,所有的风险和不确定性均难以预测,其中多数超出我们的掌控,并有可能导致我们的实际结果与我们的前瞻性陈述中表述的结果大相径庭和截然相反,其原因是各类风险因素,包括但不限于与下列因素相关的风险:我们对涉及临床结果可重复性的假设;我们对Masimo独特的无创测量技术(包括Masimo SedLine)的信念,即这些技术可对积极的临床转归及患者安全性做出贡献;与我们相信Masimo无创医学突破可提供具有成本效益的解决方案和独特优势的信念相关的风险;与COVID-19相关的风险;以及我们向美国证券交易委员会(“SEC”)递交的最新版报告中“风险因素”章节中讨论的其他因素,这些报告可从SEC的网站www.sec.gov上免费获得。尽管我们相信我们的前瞻性陈述中反映的预期是合理的,但我们并不知道我们的预期将来能否被证明正确。本新闻稿包含的所有前瞻性陈述完全符合前述警示性声明。谨此提醒您注意不要对这些前瞻性陈述给予不适当的依赖,这些陈述仅适用于今日。除非在适用的证券法律可能的要求下,我们没有任何责任来更新、修订或澄清这些陈述或是我们向SEC递交的最新版报告中包含的“风险因素”,无论是作为新信息、未来事件的结果还是其他事项的结果。
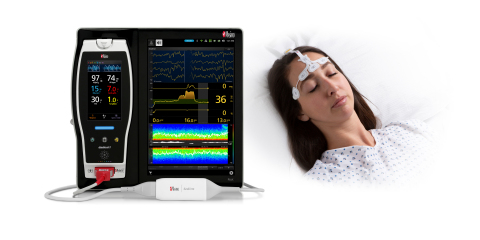
Masimo SedLine®脑功能监护仪(照片:美国商业资讯)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#神经系统#
33
#脑功能#
38
#心跳骤停#
35
#监护#
39
#ICU患者#
39
#长期生存#
33