Circ Heart Fail:肺血管疾病右心衰竭的诊断和治疗
2021-10-07 刘少飞 MedSci原创
1929 年,Werner Forssmann 对自己进行了第一次右心导管插入术,开创了使用血流动力学表征心肺功能的时代。在慢性心肺疾病患者中使用这种技术的早期研究人员认识到右心室 (RV) 对临床结
1929 年,Werner Forssmann 对自己进行了第一次右心导管插入术,开创了使用血流动力学表征心肺功能的时代。在慢性心肺疾病患者中使用这种技术的早期研究人员认识到右心室 (RV) 对临床结果的关键贡献。在过去的 20 年中,研究已经确定 RV 功能障碍是肺血管疾病 (PVD)、实质肺疾病和左心疾病患者发病率和死亡率的关键决定因素。尽管认识到这种病理生理学,但对从正常 RV 结构和功能向(不良)适应的 RV 和 RV 故障转变的时间和促成因素的机制洞察力有限。
为了解决 RV 在健康和疾病方面的理解的局限性,美国国家心肺血液研究所肺部疾病司主办了一个研讨会,以确定知识差距和研究重点,以改善 RV 的预防、预测、诊断和治疗失败,重点是 PVD 患者。各种利益相关者参加了研讨会,包括基础科学家和转化科学家;生物医学工程师;临床流行病学家和试验员;以及对血流动力学、成像、睡眠、定向治疗和网络医学感兴趣的临床医生-科学家(其他贡献者见附录)。目标是制定一项研究议程,以改善患有 RV 衰竭或具有 RV 衰竭风险的 PVD 患者的健康和结果。
右心室研究:从表型到治疗
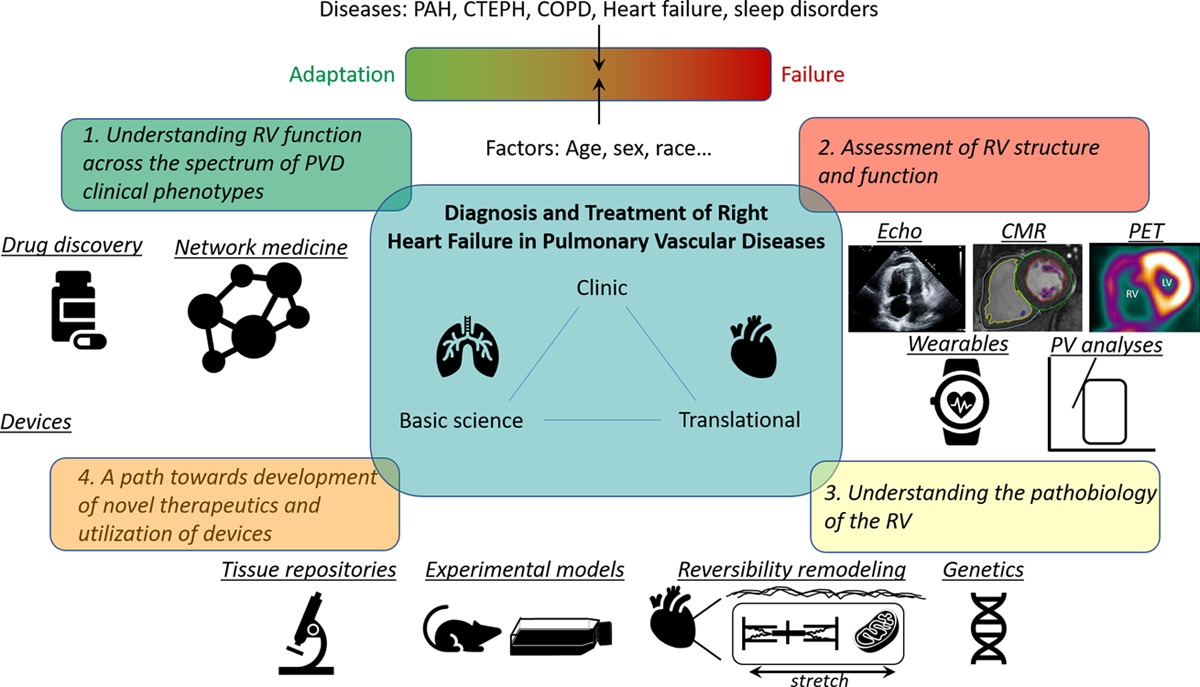
了解整个 PVD 临床表型的 RV 功能
即使在没有临床心血管疾病的成年人中,RV 的结构和功能也会因年龄、性别、种族/民族、出生时间以及产前、儿童和成人暴露而异。考虑到即使在明显健康的个体中也存在这种差异,传统的世界卫生组织肺动脉高压 (PH) 组之间和内部的 RV 形态和功能差异并不奇怪。这些区别可能归因于疾病状态本身直接对 RV 或肺血管内型后负荷的表现的影响。脉动系统中 RV 上的液压负载可能受 PVD 位置(近端与远端或两者)、血管和肺结构疾病的异质性、时间空间变异性和其他疾病特异性特征的影响。
RV 结构和功能的评估
虽然压力-容积关系被认为是评估心室功能的金标准,但这些血流动力学测量是侵入性的,目前对于大量患者的常规临床实践或研究是不切实际的。
了解 RV 的病理学
RV 的生物力学环境
RV 的代谢重编程
性、性类固醇激素和 RV 功能
临床前研究中的实验模型
新疗法开发和器械利用的途径
确定 RV 临床终点、治疗目标和治疗方法的网络医学
推进 RV 功能障碍的机械支持和干预
原始出处:
Leopold JAL.Diagnosis and Treatment of Right Heart Failure in Pulmonary Vascular Diseases: A National Heart, Lung, and Blood Institute Workshop.Circ Heart Fail. 2021 Jun;14(6):e007975
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺血管疾病#
40
#右心衰竭#
48
#右心衰#
38
#心衰竭#
36
#ART#
34
#血管疾病#
17
#HEART#
31