JACC:临床大发现:降脂还只知道“坏胆固醇”?你out了!
2021-03-19 MedSci原创 MedSci原创
他汀类药物治疗的患者,apoB和非HDL-C升高,而非LDL-C升高,与全因死亡风险和心梗风险较高相关。
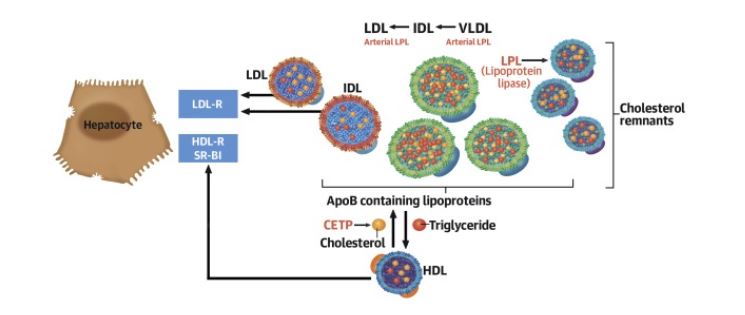
根据既往认知,大家都已认定血液中的胆固醇和甘油三酯是血脂管理的重中之重,同时可以预测心血管事件(CVD)的发生风险。其中,高密度脂蛋白(HDL)和低密度脂蛋白(LDL)是胆固醇中的一对“死对头”——LDL将脂质带到外周组织中,HDL更多是对胆固醇的反向转运,也就是不断将胆固醇从外周组织运输到肝脏。因此,LDL-胆固醇(LDL-C)一直被认为是“坏胆固醇”。
同时,动脉硬化是引发包括心肌梗死和动脉粥样硬化性心血管病(ASCVD)在内急性心血管事件的开端。因此,作为动脉硬化这一病变的核心驱动力——LDL-C是所有指南中一级与二级预防的主要治疗目标。
然而,随着研究的深入,其他血脂指标的作用也越来越受到关注,同时也出现越来越多的声音为LDL-C“平反”。
今年1月,发表在《美国心脏病学会杂志》(JACC)上的两项大型研究就激起了大家上述认知的争议:残余胆固醇,而非LDL-C或许才是引起ASCVD的罪魁祸首。这也从侧面说明,除外LDL-C,其它胆固醇指标也值得我们注意。
最近,由丹麦哥本哈根大学的专家JACC再次发表的最新研究再次支持了上述观点。研究表明,在接收降脂药——他汀类药物治疗的患者,apoB和非HDL-C升高,而非LDL-C升高,与全因死亡风险和心梗风险较高相关。
该研究总共纳入了哥本哈根市13015名接受他汀治疗的患者,进行了中位期为8年的随访。结果显示,apoB和非HDL-C升高与全因死亡和心肌梗死风险增加有关,而高LDL-C没有发现这种关联。
与apoB和非HDL-C都低于中位数患者相比:
1) apoB高于中位数而LDL-C低于中位数患者全因死亡率风险升高21%,心肌梗死风险升高49%;
2) 非HDL-C高于中位数而LDL-C低于中位数患者全因死亡率风险与心肌梗死风险则分别升高18%与78%;
3) 相反,LDL-C升高而apoB或非LDL降低则与上述风险增加无关;
4) apoB升高而非HDL-C降低的全因死亡率升高21%,但心肌梗死风险没有影响;
5) apoB和非HDL-C都高于中位数而LDL-C低于中位数的全因死亡率与心肌梗死风险分别增加23%与82%。
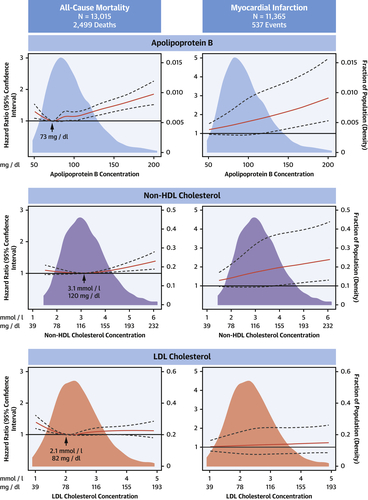
研究人员指出,在他汀类药物治疗的患者中,apoB和非HDL-C的升高,与全因死亡和心肌梗死的残余风险相关。为此,未来在心血管的二级预防中可能需要额外关注apoB的变化。
综上,在他汀治疗的患者中,apoB是比LDL-C或HDL-C更准确的全因死亡风险标志物,此外apoB也是比LDL-C更准确的心肌梗死风险标志物。
参考文献:
Apolipoprotein B and Non-HDL Cholesterol Better Reflect Residual Risk Than LDL Cholesterol in Statin-Treated Patients. J Am Coll Cardiol. 2021 Mar, 77 (11) 1439–1450
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
33
对血脂的理解上升了一个新的高度
63
#ACC#
32
学习了很多
59
里程碑式的结论么
63