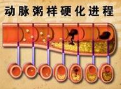
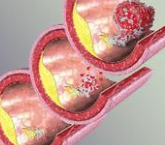
盘点:近期动脉粥样硬化相关研究进展
2016-11-07 MedSci MedSci原创
动脉粥样硬化(atherosclerosis,AS)是冠心病、脑梗死、外周血管病的主要原因,是动脉壁上沉积一层包括胆固醇结晶在内的粥样物质,使动脉弹性降低、管腔变窄,常导致心肌梗塞、中风等致命疾病发生。胆固醇结晶会引发免疫反应,导致动脉壁出现可致命的炎症。关于近期动脉粥样硬化相关研究重大成果,小M与您分享。【1】SCI TRANSL MED:预防动脉粥样硬化的新方法——补充棕榈油酸虽然脂肪类食
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#粥样硬化#
29
#相关研究#
24
小编辛苦了!为我们整理如此齐全的资料,供学习探究。点赞啦!谢谢!
51
心内科冠心病研究方向值得学习
58
心内科冠心病研究方向值得学习
74
心内科冠心病研究方向值得学习
64
心内科冠心病研究方向值得学习
63
心内科冠心病研究方向值得学习
20
心内科冠心病研究方向值得学习
23
心内科冠心病研究方向值得学习
23