Entyvio(Vedolizumab)长期维持治疗中重度活动性溃疡性结肠炎:安全性和有效性值得肯定
2020-10-12 Allan MedSci原创
武田制药有限公司今日公布了VISIBLE开放标签扩展(OLE)研究的中期结果,该研究评估了Entyvio(Vedolizumab)皮下维持治疗的长期安全性和有效性。
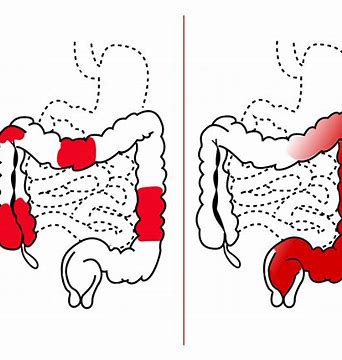
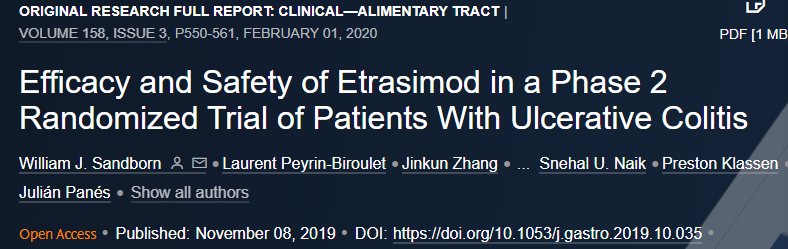
武田制药有限公司今日公布了VISIBLE开放标签扩展(OLE)研究的中期结果,该研究评估了Entyvio(Vedolizumab)皮下维持治疗的长期安全性和有效性,以治疗中度至重度活动性溃疡性结肠炎(UC)。在评估试验的主要安全性终点时,Vedolizumab的长期安全性研究结果与已知的安全性相一致。这些数据在UEG Week Virtual 2020大会上公布。
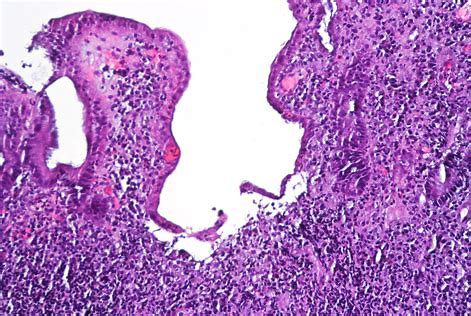
VISIBLE OLE是一项正在进行的开放标签、多中心IIIb期研究,旨在评估Entyvio(Vedolizumab)皮下维持治疗UC的长期安全性和有效性。在维持治疗的两年期间,69%的UC患者发生不良事件,最常见的不良反应分别是疾病恶化(18%)、鼻咽炎(11%)、上呼吸道感染(9%)和贫血(7%)。注射部位反应在4.5%的患者中有报道,严重程度均为轻度或中度。14%的患者发生严重不良事件,无进行性多灶性白质脑病病例,无死亡病例。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















维得利珠真是一个好药
62
#活动性溃疡性结肠炎#
31
学习了
86
#安全性和有效性#
34
#Entyvio#
36
#溃疡性#
29
#mAb#
22
好
77
#活动性#
27
#vedolizumab#
35