Cell Death Dis:lncRNA DLGAP1-AS1促进肝癌发生发展及上皮-间质转化
2020-04-05 MedSci原创 MedSci原创
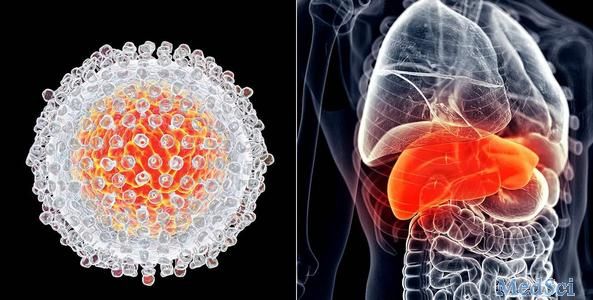
肝细胞癌(HCC)是世界上最常见且致命的恶性肿瘤之一,而上皮-间质转化(EMT)进程是影响HCC发生发展及转移的关键因素。在既往研究中,长链非编码RNA(lncRNA)已被证实可以充当各种肿瘤生物过程
在该研究中,研究人员阐明了lncRNA DLGAP1-AS1在调节肝细胞癌的发生发展以及EMT中的一些潜在的功能和机制。该研究显示DLGAP1-AS1在HCC细胞系中表达水平被上调并且能够促进HCC的发生发展及EMT进程。
此外,DLGAP1-AS1被证明可以用作竞争性分子海绵,通过结合抑制HCC抑制性的miRNA,miR-26a-5p和miR-26b-5p,从而提高致癌细胞因子IL-6的表达水平;而IL-6可以激活JAK2/STAT3信号通路并且与DLGAP1-AS1相互激活彼此的转录活性,从而形成了一个正反馈环路。此外,研究人员发现DLGAP1-AS1在HCC细胞中的致癌作用主要通过正向调控miR-26a/b-5p的下游基因CDK8和LRP6,从而激活Wnt/β-catenin信号通路来实现的。
总而言之,该研究结果阐明了DLGAP1-AS1在体内体外促进HCC发生发展及EMT进程的详细分子机制,并提示DLGAP1-AS1或可作为HCC治疗的潜在靶标。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
32
#Cell#
32
#CRN#
33
#Dis#
41
#发生发展#
30
#lncRNA#
31
#Death#
32
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
39