European Radiology:US计算机辅助诊断系统在鉴别乳腺肿块良恶性方面的价值
2022-06-03 shaosai MedSci原创
超声(US)检查不仅可以作为乳腺钼靶检查的辅助手段,也可以单独作为一种影像学筛查手段来提高乳腺恶性肿块的检测率。
 2020年,乳腺癌是全球女性癌症中新发和死亡的主要原因,早期发现和及时诊断对乳腺癌的治疗和预后都很重要。
2020年,乳腺癌是全球女性癌症中新发和死亡的主要原因,早期发现和及时诊断对乳腺癌的治疗和预后都很重要。
超声(US)检查不仅可以作为乳腺钼靶检查的辅助手段,也可以单独作为一种影像学筛查手段来提高乳腺恶性肿块的检测率。然而,US的局限性在于对操作者的依赖性和对乳腺肿块的分类缺乏特异性,导致观察者之间的差异性和不必要的组织活检。乳腺成像报告和数据系统(BI-RADS)由美国放射学会于2003年提出,用于规范放射科医生的乳房超声报告,目前已更新至第五版、。BI-RADS分类有7个类别,其中第4类的恶性概率范围最广,从3%到94%,建议进行活检。研究表明,第4类不足以区分良性和恶性乳腺肿块,这可能会增加不必要的活检需要。
目前,计算机辅助诊断(CAD)系统已应用于超声检查的辅助诊断。作为基于深度学习算法的商用CAD软件,S-Detect(Samsung Ultrasound RS80A, Samsung Medison Co. Ltd.)已被用于乳腺和甲状腺病灶的分类。据我们所知,目前还没有一项多中心研究来探讨S-Detect软件在乳腺肿块分类和避免不必要的活检方面的诊断价值。
近日,发表在European Radiology杂志的一项研究评估了CAD软件在区分良性和恶性乳腺肿块和避免不必要的活检方面的诊断价值,为提高乳腺癌的检出率及诊断准确性提供了技术支持。
本项前瞻性的多中心研究纳入了2019年4月至2020年11月期间预定进行乳腺肿块病理诊断的患者,获得了每位患者超声图像、视频、CAD分析和BI-RADS并计算了AUC、准确性、敏感性、特异性、PPV和NPV,并与放射科医生的诊断结果进行了比较。
共有901名患者的901个乳腺肿块被纳入了研究。CAD软件的准确性、敏感性、特异性、PPV和NPV在长轴部分分别为89.6%、94.2%、87.0%、80.4%和96.3;在短轴部分分别为89.0%、91.4%、87.7%、80.8%和94.7%。以BI-RADS 4a为分界值,CAD软件的AUC(0.906 vs 0.734 vs 0.696,均P<0.001)高于有经验和经验不足的放射科医生。以BI-RADS 4b为临界值,CAD软件显示出比经验不足的放射科医生更好的AUC(0.906 vs 0.874,p < 0.001),但不优于经验丰富的放射科医生(0.906 vs 0.883,p = 0.057)。应用CAD软件后,BI-RADS 4类和5类的不必要活检率明显下降(33.0% vs 11.9%,37.8% vs 14.5%),4a类活检的恶性率明显上升(11.6% vs 40.7%,7.4% vs 34.9%,P均<0.001)。
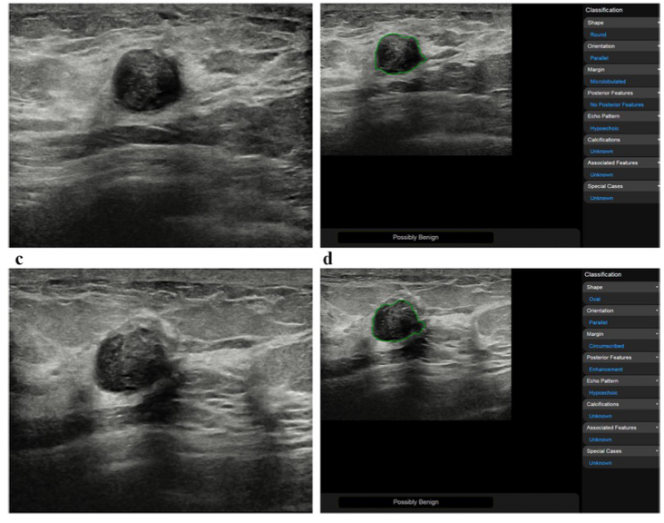
图 53岁女性,患有乳腺肿块,病理结果为良性增生性疾病。乳腺肿块短轴切面的B型超声图像(a)和相应的CAD软件分析显示 "可能为良性"(b),长轴切面的B型超声图像(c)和相应的CAD软件分析显示 "可能为良性"(d)
本项多中心研究表明,CAD软件可作为一种鉴别良性和恶性乳腺肿块的非侵入性的影像学技术,可能用作乳腺肿块诊断的有效辅助诊断工具,并实现不必要活检的减少。
原文出处:
Qi Wei,Yu-Jing Yan,Ge-Ge Wu,et al.The diagnostic performance of ultrasound computer-aided diagnosis system for distinguishing breast masses: a prospective multicenter study.DOI:10.1007/s00330-021-08452-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#计算机#
46
#PE#
32
#乳腺肿块#
45
#肿块#
47