J Thromb Haemost:血栓调节蛋白 (THBD) 基因变异与血栓形成风险
2022-01-05 MedSci原创 MedSci原创
罕见的符合条件的THBD突变与VTE相关,表明THBD中的罕见变异会促进VTE的发生发展。
血栓调节蛋白(TM)是在1980年代发现的,当时人们认识到酶原蛋白C(PC)被凝血酶转化为活化蛋白C(APC)。PC抗凝系统在调节止血中起关键作用。尽管几项研究已经在静脉血栓栓塞(VTE)患者中发现了血栓调节蛋白基因(THBD)变异,但THBD在VTE患者中的作用仍有待阐明。

近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,该研究旨在明确大型中老年人群中罕见和常见THBD变异个体的血栓形成风险。
研究人员对参与马尔默饮食与癌症研究(1991-1996)的28794名受试者(出生于1923-1950年,60%为女性)的THBD外显子组序列进行了合格突变分析。从基线开始对患者进行随访,直到第一次发生VTE、死亡或2018年。合格突变被定义为功能丧失或非良性(PolyPhen-2)错义变异,次要等位基因频率<0.1%。
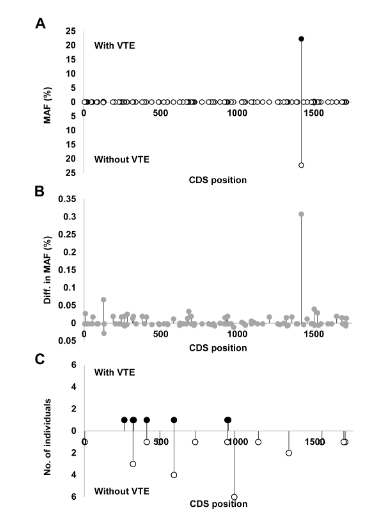
研究人员发现单个常见编码突变rs1042579与VTE事件无关。16种罕见突变被归类为合格并纳入折叠分析。七名患有VTE的个体与24名没有VTE的个体相比,携带一种合格的变异。针对年龄、性别、体重指数、收缩压、吸烟和饮酒、rs6025、rs1799963以及来自PCA分析的前两个特征向量进行调整的Cox多元回归分析显示对于罕见的合格突变风险比为3.0(95%CI1.4-6.3)。THBD中合格突变的分布在发生和没有发生VTE的个体中存在差异,这表明可能存在位置效应。
由此可见,罕见的符合条件的THBD突变与VTE相关,表明THBD中的罕见变异会促进VTE的发生发展。
原始出处:
Eric Manderstedt.et al.Thrombomodulin (THBD) gene variants and thrombotic risk in a population-based cohort study.Journal of Thrombosis and Haemostasis.2022.https://onlinelibrary.wiley.com/doi/10.1111/jth.15630
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#HAE#
53
#血栓调节蛋白#
44
#血栓#
73
#基因变异#
51
#变异#
39
学习
55
学习
68
先收藏
63