Radiology:内皮剪切应力与冠状动脉CTA斑块特征及PET血管舒张功能的关系
2021-08-21 shaosai MedSci原创
冠状动脉CT血管成像(CCTA)是临床上广泛使用的评估冠状动脉解剖结构的非侵入性成像方式。
 冠状动脉CT血管成像(CCTA)是临床上广泛使用的评估冠状动脉解剖结构的非侵入性成像方式。快速的技术改进使得评估冠状动脉粥样硬化斑块的表型和负担成为可能,计算流体力学和三维重建技术的进步可实现通过评估CT分数流量储备或类似指标来评估冠状动脉病变的功能意义。
冠状动脉CT血管成像(CCTA)是临床上广泛使用的评估冠状动脉解剖结构的非侵入性成像方式。快速的技术改进使得评估冠状动脉粥样硬化斑块的表型和负担成为可能,计算流体力学和三维重建技术的进步可实现通过评估CT分数流量储备或类似指标来评估冠状动脉病变的功能意义。
现阶段,在CCTA中评估血管壁的生物力学特征是一项逐渐被人们所认识及关注的方面。其中内皮剪切应力(ESS)是动脉壁附近动态黏度和血流速度梯度的产物,在冠状动脉斑块的形成和发展中起着关键作用。另外,冠状动脉血管扩张高峰期的血流增加会造成局部ESS的增加,该现象在动脉粥样硬化病变中更加明显。然而据我们所知,尚未有呀扭探讨过解剖学、形态学和生物力学数据与心肌血流之间的复杂关系。
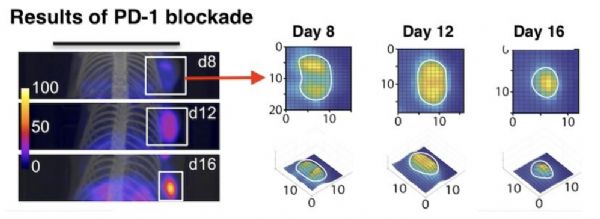
近日,发表在Radiology杂志的一项研究评估了计算流体力学指标、冠状动脉病变的解剖学和形态学特征之间的关系,以及它们在使用PET心肌灌注成像(MPI)评估冠状动脉血管舒张能力受损方面的性能比较,为临床提供更有价值的评估心肌血流受损的预测因素。
本项研究于 2019年10月至2020年9月期间分析了同时接受CCTA和PET MPI检查并对心肌血流进行量化的稳定胸痛和冠状动脉疾病患者的冠状动脉。CCTA图像用于评估狭窄的严重程度、病变特定的总斑块体积(PV)、非钙化的PV、钙化的PV和斑块表型。PET MPI被用于评估明显的冠状动脉狭窄。通过使用接收器操作特征曲线下的面积(AUC)分析,评估了CCTA衍生参数的预测性能。
共对53名患者(平均年龄65岁±7岁;31名男性)的92条冠状动脉血管进行了评估。狭窄程度大于50%的病变与没有明显狭窄的病变相比,ESS更高(平均,15.1 Pa ± 30 vs 4.6 Pa ± 4 vs 3.3 Pa ± 3;P = .004)。功能显著的病变与不显著的病变相比,ESS更高(中位数,7 Pa [四分位数范围,5-23 Pa] vs 2.6 Pa [四分位数范围,1.8-5 Pa],分别;P≤.001)。将ESS添加到狭窄严重程度评估中可提高对功能显著病变的预测(AUC变化,0.10;95%CI:0.04,0.17;P = .002)。
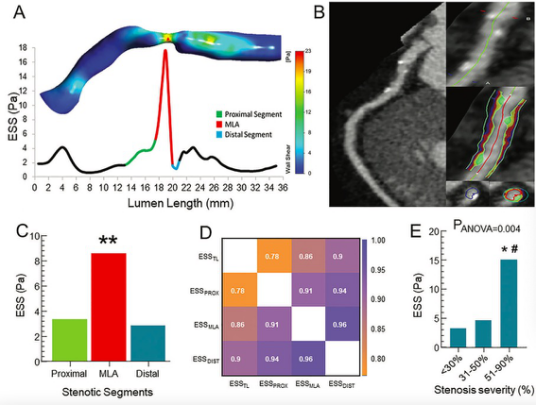
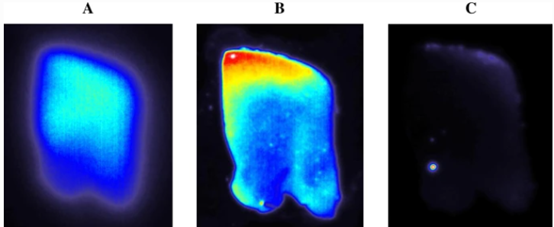
图1 内皮层剪切应力(ESS)狭窄段、斑块分析和狭窄严重程度。(A) 64岁男性患者的右冠状动脉切面,在血管长度上计算出的平均ESS段(0.5mm间隔)。与近端和远端段相比,最小腔面积(MLA)显示出更高的平均ESS值(10 Pa vs 3.6 Pa vs 1.8 Pa)。(B)冠状动脉CT血管造影(左图)和弧形平面重塑(右上图)的左前降支动脉斑块识别;感兴趣容积处特写和斑块成分的颜色叠加(右中图;蓝色,坏死核心[30至30HU];红色,纤维脂肪[31-130HU];黄色,纤维性[131-350HU];绿色,致密钙[350HU])。横断面图(右下角)显示了腔内边界,并对个别斑块成分进行了颜色叠加。(C) 分段病变中平均ESS值的分布。近端段的ESS值比远端段高。最小腔面积(MLA)在三个计算的狭窄段中显示最高的ESS值。与近端和远端相比,**P .05。(D) 相关矩阵显示了总病变(ESSTL)、近端(ESSPROX)、最小腔面积(ESSMLA)和远端节段(ESSDIST)的ESS之间的相关性。(E) 最小腔面积ESS在狭窄严重程度上的平均分布。
本研究表明,内皮层剪切应力(ESS)与冠状动脉斑块的体积和管腔狭窄的严重程度呈正相关。此外,斑块的解剖结构和ESS所捕捉到的流体动力学变化似乎是冠状动脉病变功能显著的重要信息。此外,ESS可以通过改善对使用PET心肌灌注成像评估的血管扩张能力受损的预测,为狭窄的严重程度提供附加价值。
原文出处:
Georgios-Eleftherios Kalykakis,Alexios S Antonopoulos,Thomas Pitsargiotis,et al.Relationship of Endothelial Shear Stress with Plaque Features with Coronary CT Angiography and Vasodilating Capability with PET.DOI:10.1148/radiol.2021204381
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#冠状动脉CT#
27
#舒张功能#
24
#CTA#
30
#剪切应力#
39
#PE#
25
#血管舒张#
42
#斑块#
23
#PET#
30
#应力#
39