Neuroradiology:高灌注引起的脑梗死?还是脑梗死后高灌注?
2019-05-31 佚名 脑血管病及重症文献导读
65岁,女性。既往高血压病史。因为突发表达性失语就诊,无其他神经功能缺损。
65岁,女性。
既往高血压病史。
因为突发表达性失语就诊,无其他神经功能缺损。
CT 未见颅内出血,CTA 未见血管闭塞。
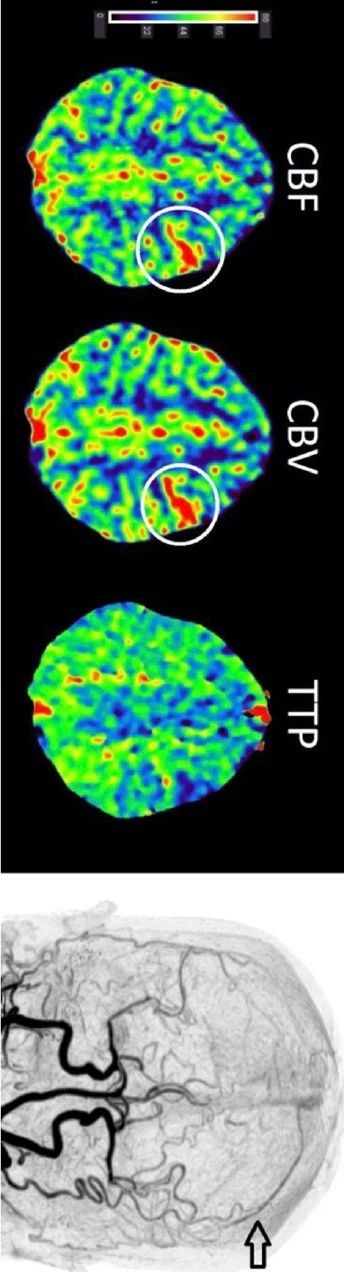
CT 灌注显示左侧额叶皮层小片灌注异常,CBF 和 CBV增加,为高灌注表现(下图)。CTA(dynamic subtraction CTA rendering of CT perfusion)显示皮层静脉提前充盈(early contrast filling)。不除外动静脉分流:
随后头 MRI 显示相应区域弥散受限,符合缺血的表现(下图):
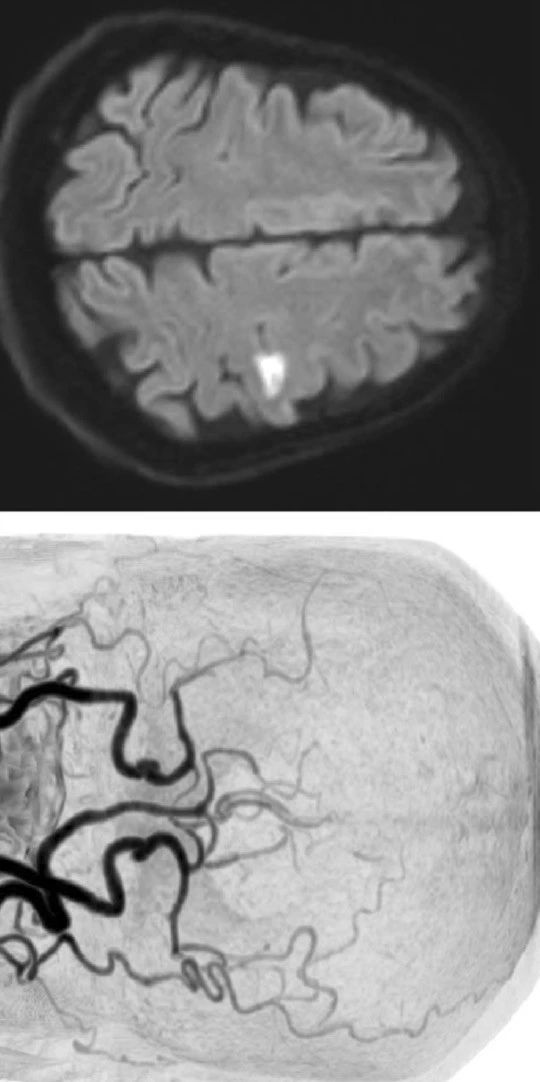
MRA 未见明显异常。
患者症状患者,随访也未发生其他新的症状。给予氯吡格雷和辛伐他汀治疗。
6周后随访4D-CT 未见任何异常,无 AV 分流的征象。
原始出处:Anna Koopman, Frank-Erik de Leeuw, Frederick Meijer. CT perfusion hypervolemia: brain ischemia or stroke mimic? Neuroradiology. April 2019
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#高灌注#
46
#脑梗#
32
学习了,谢谢
89