用光打开血脑屏障:脑部给药的新方法
2021-12-22 brainnew神内神外 网络
美国得克萨斯大学达拉斯分校的秦真鹏教授团队和美国得克萨斯大学西南医学中心的Robert Bachoo教授团队共同研发了一种通过皮秒脉冲激光照射分子靶向的纳米颗粒来实现安全可逆地打开血脑屏障并传送药物到
指导 | 秦真鹏 教授
说明 | 本文来自课题组(论文作者)投稿
血脑屏障(名词解释>)是存在于血液和脑组织之间的一种具有保护性的生理屏障。血脑屏障通过只让氧气等必须物质入脑且防止血液有害物质侵入,从而维持中枢神经系统稳态,并保护脑部组织免受代谢产物损伤。
但与此同时,脑部疾病的治疗极具挑战,最主要的障碍之一就是血脑屏障限制了98%的小分子药物和几乎全部大分子药物无法有效到达脑部病灶。因此,如何安全可逆地打开血脑屏障让药物进入脑组织,是中枢神经系统疾病治疗的研究热点,并具有重要的临床意义。
目前用于增加血脑屏障通透性的方法主要分为两类:
一类是增加脑半球或是全脑血脑屏障通透性,包括颈动脉注射高浓度甘露醇,血管活性试剂激活胞吞作用,以及通过利用细胞穿透肽、可穿透血脑屏障的腺病毒相关病毒(AAV)以及受体介导的转胞吞作用来增加脑转运。这些方法适合需要全脑治疗的疾病,如老年痴呆症,但不适合只需要局部治疗的疾病,比如早期脑肿瘤。
另一类是通过超声刺激微泡来实现局部增加脑渗透,该方法已经在进行早期临床试验,具有很大的应用前景。然而超声方法对于应用在复杂骨结构下面的组织具有局限性,例如脊柱下面的血脊屏障。
鉴于此,美国得克萨斯大学达拉斯分校的秦真鹏教授团队和美国得克萨斯大学西南医学中心的Robert Bachoo教授团队共同研发了一种通过皮秒脉冲激光照射分子靶向的纳米颗粒来实现安全可逆地打开血脑屏障并传送药物到脑组织里面的技术(图1)。
相关工作以“Reversibly Modulating the Blood-Brain Barrier by Laser Stimulation of Molecular-Targeted Nanoparticles”为题发表在Nano Letters上,并被选为封面论文。

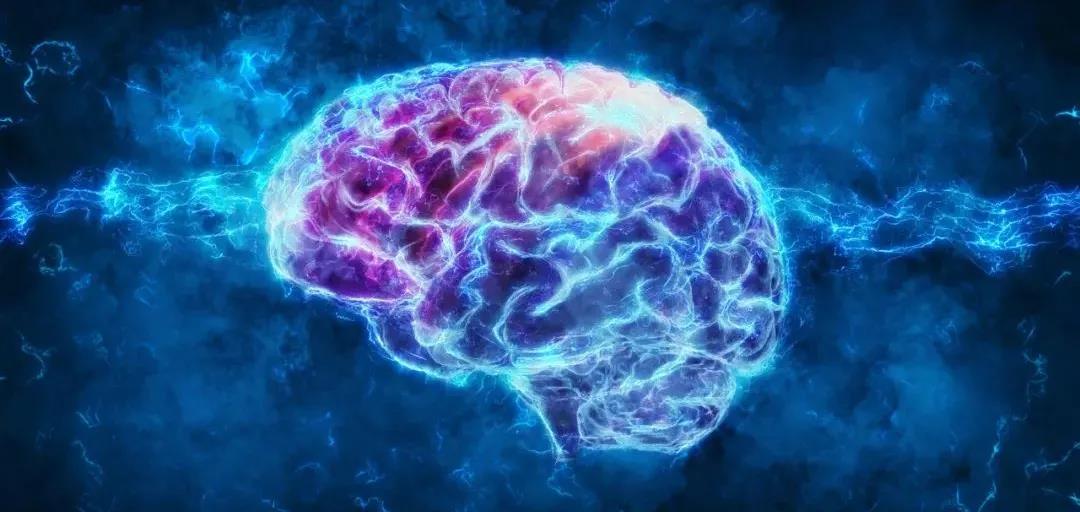
图1:皮秒脉冲激光照射分子靶向的金纳米颗粒打开血脑屏障实现药物递送的艺术效果图。
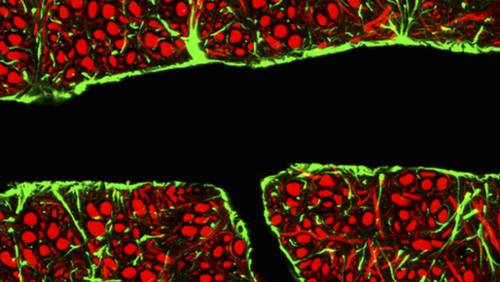
此技术原理利用皮秒激光刺激靶向金纳米颗粒后会在其周围纳米范围内产生很小的机械波,并作用在血脑屏障的紧密链接(名词解释>)(由多种链接蛋白组成的复合体构成一道物理屏障来防止各种分子透过从而密封相连细胞间的间隙)上从而打开血脑屏障。
在此项工作中,研究人员首先合成了金纳米颗粒,并通过抗体修饰,使其可以靶向紧密链接复合体的其中一种连接黏附分子A蛋白(JAM-A)。把修饰后的颗粒经尾静脉注射进小鼠后,用皮秒激光在头颅上方照射一个脉冲,就可以打开部分紧密连接从而增加血脑屏障的通透性。
相对于传统的打开血脑屏障的技术,本文所提出的方法的优势体现在如下几个方面:
(1)具有高时间-空间分辨率和可逆性。该研究表明,只有在皮秒激光照射和分子靶向的金纳米颗粒同时存在的情况下,才可以打开小鼠的血脑屏障。并且在低能量下血脑屏障通透性在数小时内恢复正常。
(2)具有良好的安全性。研究人员发现,用激光打开血脑屏障不会影响小鼠脑部自发性的血管舒缩。同时,脑血管密度,血管上葡萄糖转运体以及脑实质内多种重要细胞结构 (例如神经元核抗原,轴突初始段蛋白、壁细胞星形胶质细胞足突上的水转运体和周细胞的神经胶质抗原2)在激光处理前后没有显著性差异。
(3)可以实现高效传输药物到脑实质里。该研究证实,此项技术可以将典型的药物如抗体IgG(14 nm),基因治疗载体AAV (26 nm)以及药物载体脂质体(80 nm)有效输送至脑实质里 (图2)。
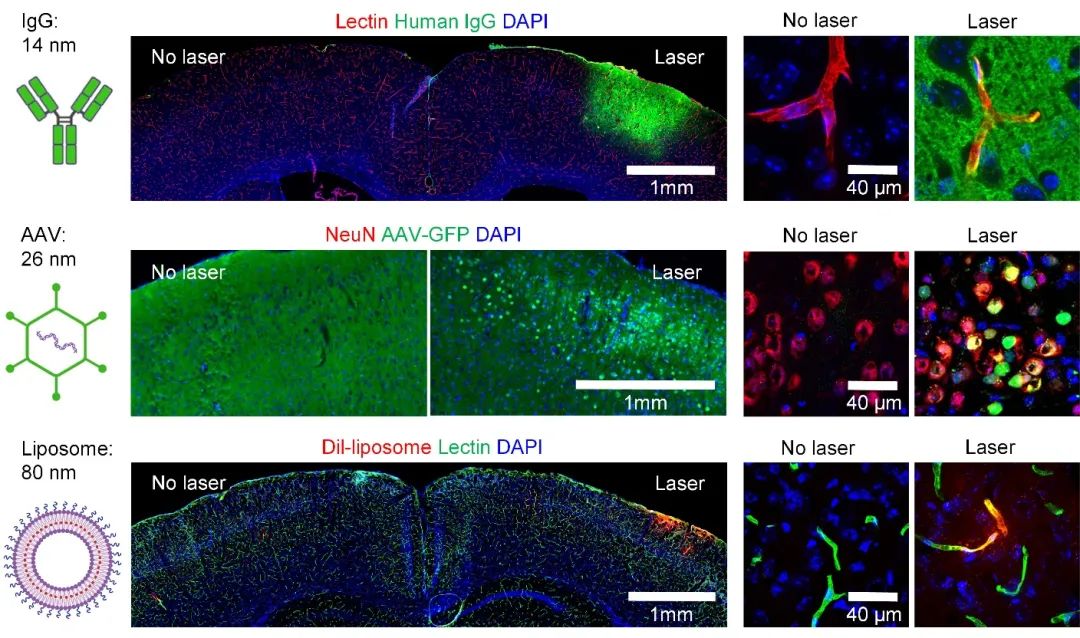
图2:血脑屏障通透性增加来递送抗体(IgG),基因治疗载体 (AAV)和脂质体到脑实质。
血脑屏障是中枢神经系统疾病治疗需要攻克的一道难关,找到安全并且高效地打开血脑屏障的方法是科研人员多年来主要的研究目标之一。
综上,本文所提出的用光打开血脑屏障的方法是可逆的,且不会破坏神经血管结构,因此在中枢神经系统的疾病(例如脑肿瘤,渐冻症以及中风)的治疗中具有广泛的应用前景。
论文信息:
Nano Lett. 2021, 21, 9805−9815
https://doi.org/10.1021/acs.nanolett.1c02996

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新方法#
35
有意思!
50
这个很有意思
49
#血脑屏障#
39
受益匪浅
0