BMC Gastroenterology:Cyr61的表达水平与克罗恩病患者的临床病程有关
2021-03-24 MedSci原创 MedSci原创
克罗恩病(CD)是一种特发性的慢性肠道炎症,会影响人们消化系统的各个部分。为了保持正常的炎症与修复的动态平衡,机体需要在组织受伤或生理损伤后进行修复。
克罗恩病(CD)是一种特发性的慢性肠道炎症,会影响人们消化系统的各个部分。为了保持正常的炎症与修复的动态平衡,机体需要在组织受伤或生理损伤后进行伤口愈合过程。富含半胱氨酸血管生成诱导61(Cyr61,CCN1)是一种可以分泌肝素并结合细胞外基质相关蛋白和影响细胞粘附和细胞迁移的重要调节剂。先前的研究表明,炎症性肠病患者和实验性结肠炎小鼠的结肠黏膜中Cyr 61的水平明显升高,表明Cyr61参与了结肠炎模型的发病过程。因此,这项研究中旨在探讨CD患者中Cyr61的结肠黏膜表达,并分析Cyr61表达与临床疾病活动和/或预后之间的关系。

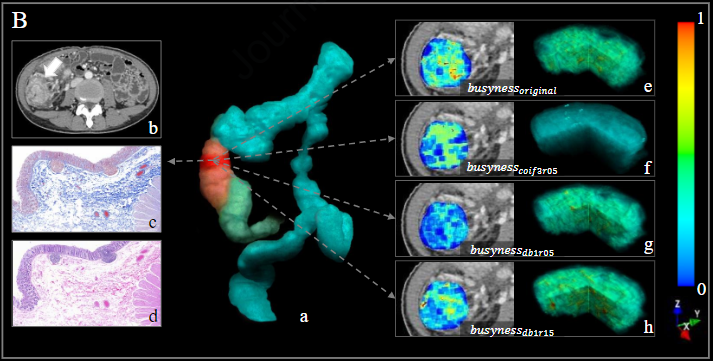
研究人员从病例数据库中筛选了83例CD患者和372例对照组患者的内窥镜样本,通过免疫组织化学(IHC)比较患者粘膜中Cyr61的表达。CD患者Cyr61表达的IHC评分分为三分位数,以评估其与临床病程的相关性。研究人员还测量了CD患者发炎和未发炎的结肠黏膜病变中Cyr 61和促炎基因的mRNA水平。
CD患者中Cyr61表达的平均IHC评分明显高于对照组(86.5 VS 46.1,P <0.001)。在CD患者中,临床复发患者的Cyr61表达平均IHC评分低于无复发患者(68.3 VS 92.2,P = 0.01)。 CD患者有炎症的黏膜中Cyr61 mRNA水平是非发炎性病变的两倍(P > 0.05),发炎的黏膜中IL-6和TLR-4的mRNA水平显着高于未发炎的黏膜(P <0.05)。当CD患者根据IHC Cyr61表达评分分为三分位数组时,Cyr61高表达患者的临床复发率往往较低(P= 0.02)。与Cyr61的高表达临床复发风险降低相关(OR 0.43,95%CI 0.20–0.92,P = 0.03)。

CD患者中Cyr61粘膜表达与临床病程呈负相关,研究人员认为Cyr 61在CD患者中激活炎症反应,促进伤口愈合和组织修复中发挥重要作用。
原始出处 :
Su-Mi Lee. Et al. Expression of Cyr61 is associated with clinical course in patients with Crohn’s disease. BMC Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Gastroenterol#
36
#临床病程#
38
#GAS#
23
#BMC#
49
#表达水平#
34
学习了,很受益
69
#AST#
23
#Gastroenterology#
20
已学习
75