Int Urogynecol J:尿液生物标志物在女性膀胱过度活动症诊断中的应用
2021-08-15 AlexYang MedSci原创
根据国际尿控协会(ICS)和国际妇科泌尿协会(IUGA)的定义,
根据国际尿控协会(ICS)和国际妇科泌尿协会(IUGA)的定义,膀胱过度活动症(OAB)综合症是一种慢性膀胱临床疾病,包括尿急,通常伴有尿频和夜尿,伴有或不伴有急迫性尿失禁,且没有尿路感染或其他明显病变。神经生长因子(NGF)、脑源性神经营养因子(BDNF)和其他蛋白与膀胱过度活动症(OAB)综合征有关,因为它们的尿液浓度与一般非OAB人群的浓度有明显差异。

近期,有研究人员系统地评估了NGF、BDNF和其他尿液副产物是否可以作为潜在的生物标志物来管理OAB女性患者。
研究是一个根据PRISMA指南进行的系统回顾和元分析。研究人员对Medline、Scopus、ScienceDirect、Embase和Cochrane Register数据库进行了搜索,鉴定了2020年10月之前的研究。纳入的研究调查了OAB与NGF、BDNF和其他潜在生物标志物在有症状的妇女及其对照组中的相关性。
研究共纳入了12项研究(581名女性OAB患者和394名女性对照组)。尿液中的NGF、NGF/Cr、BDNF/Cr、ATP/Cr和PGE2/Cr的比率确定为女性OAB患者的潜在生物标志物。元分析的结果表明,uNGF[标准平均差(SMD)1.45,95%CI 0.53-2.36]、NGF/Cr比率(SMD 1.23,95%CI 0.67-1.78)、BDNF/Cr比率(SMD 0.78,95%CI 0.006-1.50),以及BDNF/Cr比率(RR 0.78,95% CI 0.006-1.50)在女性OAB患者中与健康对照组相比有所增加,而PGE2/Cr和ATP/Cr比率没有发现差异。在女性患者OAB的管理中,目前的数据不足以评估任何其他潜在的生物标志物,如尿液中的MDA、ATP和细胞因子。
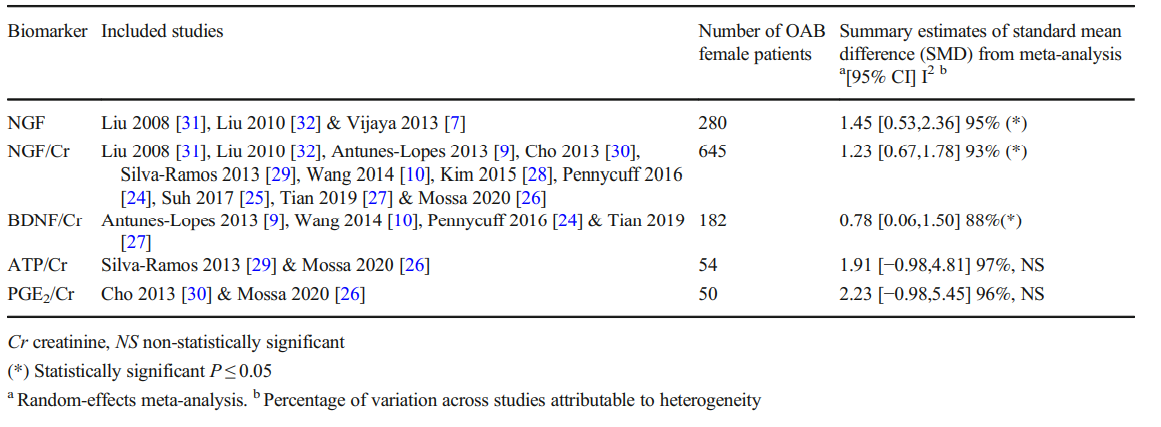
元分析结果
综上所述,uNGF、NGF/Cr和BDNF/Cr比率可用于评估女性OAB患者。但仍旧需要进一步的研究来明确OAB亚组和健康妇女的OAB尿液滴度水平,以及它们作为OAB妇女诊断和管理工具的潜力。
原始出处:
Sofia Tsiapakidou , Apostolos Apostolidis , Konstantinos Pantazis et al. The use of urinary biomarkers in the diagnosis of overactive bladder in female patients. A systematic review and meta-analysis. Int Urogynecol J. Aug 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#膀胱过度活动症#
52
#NEC#
39
#标志物#
44
#尿液#
49
#生物标志#
43
#生物标志#
35