NAT MED:阿特珠单抗治疗尿路上皮癌的临床疗效和生物标志物分析
2019-11-09 海北 MedSci原创
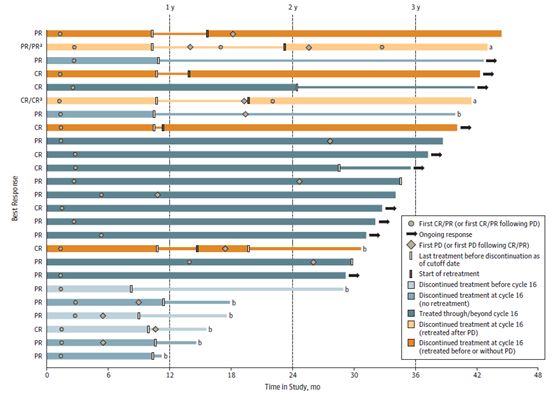
最近,研究人员进行了一项单臂2期临床研究,该研究包括了95例具有肌肉浸润性尿路上皮癌的患者,其在膀胱切除术前接受了两个周期的atezolizumab治疗(ClinicalTrials.gov标识符:NCT02662309)。
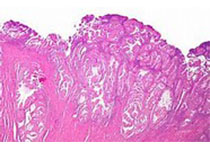
靶向PD-1或其配体PD-L1的抗体(例如atezolizumab)能够在一部分转移性尿路上皮癌中具有良好功效。生物标志物可能有助于鉴定这些反应性肿瘤的特点。
这些药物的新辅助使用与包括尿路上皮癌在内的一系列肿瘤的病理完全缓解有关。这些研究的连续组织采样使得研究人员能够进行详细的生物标志物的分析。
最近,研究人员进行了一项单臂2期临床研究,该研究包括了95例具有肌肉浸润性尿路上皮癌的患者,其在膀胱切除术前接受了两个周期的atezolizumab治疗(ClinicalTrials.gov标识符:NCT02662309)。
病理完全缓解是主要终点。次要研究终点是安全性,无复发生存和生物标志物分析。
结果显示,给药之后,病理完全缓解率为31%(95%置信区间:21–41%),达到了主要疗效终点。基线生物标志物显示,预先存在的活化T细胞的出现比预期的更为突出,并且与临床结果相关。
其他已建立的生物标志物,例如肿瘤突变负荷,不能预测临床结果,这与转移情况有所不同。
基因表达特征和蛋白质生物标志物的动态变化随治疗发生,而DNA随治疗变化的改变并不常见。
响应的肿瘤在治疗后显示出与组织修复相关的基因的高表达,这使得该组中对肿瘤生物标志物的解释具有挑战性。诸如转化生长因子-β和成纤维细胞活化蛋白之类的基质因子与抗药性有关,处理后细胞周期基因标记的高表达也与抗药性相关。
原始出处:
Thomas Powles et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nature Medicine, 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#标志物#
40
#Nat#
0
#临床疗效#
24
#上皮癌#
24
#生物标志#
31
#生物标志#
33
#Med#
24
谢谢梅斯提供这么好的信息,学到很多
37