Ann Neurol:Covid-19患者Guillain-Barré综合征的发病率、临床特征、危险因素和结局
2020-12-12 MedSci原创 MedSci原创
SARS-CoV-2可能是另一种引起GBS的病毒。
近日,神经病学领域权威取杂志Annals of Neurology上发表了一篇研究文章,研究人员旨在评估Covid-19患者患Guillain-Barré综合征(GBS)的发病率、临床特征、危险因素和结局。
在Covid-19大流行期间,研究人员从在西班牙61个急诊(ED)就诊的71904名COVID患者中诊断出11例格林-巴利综合征(GBS)患者。
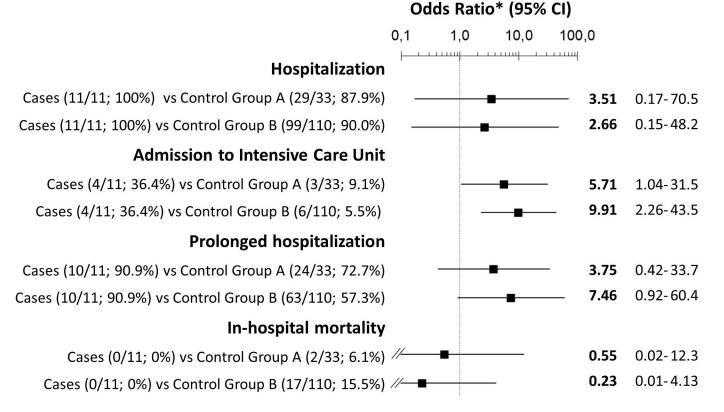
研究人员发现ED患者中GBS的相对频率在COVID患者(0.15‰)中高于非COVID患者(0.02‰)(OR=6.30,95%CI=3.18-12.5),其标准化发生率也是如此(分别为9.44和0.69例/100000,OR=13.5;95%CI=9.87-18.4)。就临床特征而言,COVID伴GBS患者的嗅觉-味觉障碍比非COVID伴GBS(OR=27.59,95%CI=1.296-587)和COVID-non-GBS患者(OR=7.875,95%CI=1.587-39.09)更为频繁。尽管COVID-GBS患者更常接受重症监护,但与对照组相比,死亡率并未增加。
该研究结果表明,SARS-CoV-2可能是另一种引起Guillain-Barré综合征的病毒。
原始出处:
Marcos Fragiel,et al.Incidence, clinical characteristics, risk factors and outcomes of Guillain‐Barré syndrome in patients with Covid‐19.Annals of Neurology.2020.https://onlinelibrary.wiley.com/doi/10.1002/ana.25987
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Neurol#
0
#临床特征#
33
#发病率#
26
#COVID-19患者#
32
#综合征#
32
学习了
73
受教了
85