AACE2019:2型糖尿病可使老年女性短期骨折风险加倍
2019-05-07 国际糖尿病编辑部 国际糖尿病
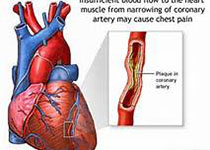
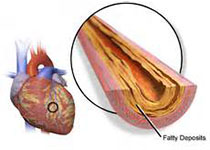
2型糖尿病(T2DM)是引起骨骼损伤以及骨脆性增加的独立危险因素。在刚刚结束的第28届美国临床内分泌医师协会年会(AACE2019)上,一项基于弗雷明汉姆研究初始受试者及其后代队列(Framingham Original and Offspring Cohorts)进行的分析显示,在1年内,T2DM女性患者的骨折风险是无糖尿病女性的两倍!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ACE#
32
#AACE#
25
#ACE2#
26
#骨折风险#
23
谢谢MedSci提供最新的资讯
33