ASCO GU 2021:上尿路尿路上皮癌的术后辅助化疗III期POUT试验结果更新
2021-02-16 MedSci原创 MedSci原创
上尿路尿路上皮癌(UTUC)包括肾盂癌和输尿管癌,与膀胱癌同属尿路上皮癌。UTUC发病年龄多为50~70岁,占全部尿路上皮癌的5%~10%,而在中国这一比例可能更高,且肿瘤侵袭性高、预后差,术后仍有2
上尿路尿路上皮癌(UTUC)包括肾盂癌和输尿管癌,与膀胱癌同属尿路上皮癌。UTUC发病年龄多为50~70岁,占全部尿路上皮癌的5%~10%,而在中国这一比例可能更高,且肿瘤侵袭性高、预后差,术后仍有22%~47%的患者在随访期间出现膀胱内复发。对于接受根治性的肾输尿管切除术的UTUC患者,术后辅助化疗能否获益在国际上尚无定论。POUT研究是一项针对UTUC患者术后接受辅助化疗与观察对比的多中心随机对照Ⅲ期临床试验,该研究旨在评估基于铂类药物的全身化疗对UTUC患者的临床获益。去年研究结果发表在Lancet上,此次更新了新的随访结果。
研究设计
POUT试验(CRUK / 11/027; NCT01993979)先前曾报道,经组织学证实为pT2-T4 N0-3 M0上尿路尿路上皮癌的患者,辅助化疗可改善无病生存期(HR 0.45,95%CI 0.30-0.68)。中位随访时间为30.3个月。1在GU ASCO 2021年会上,Alison Birtle博士及其同事介绍了一项预先计划的分析结果,该报告更新了无病生存的主要终点并报告了包括总体生存在内的主要次要终点。
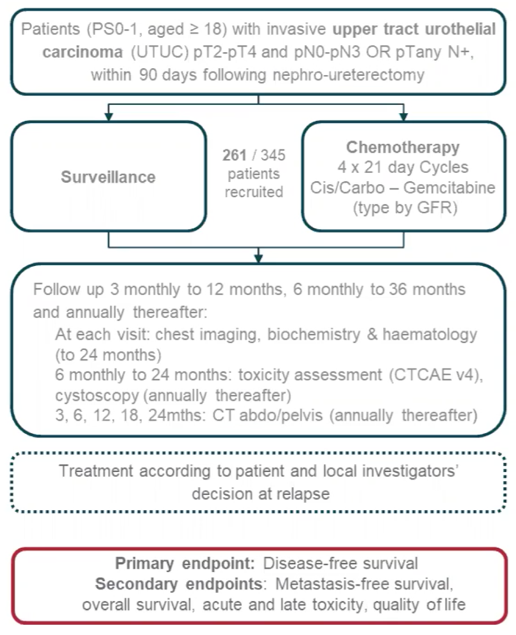
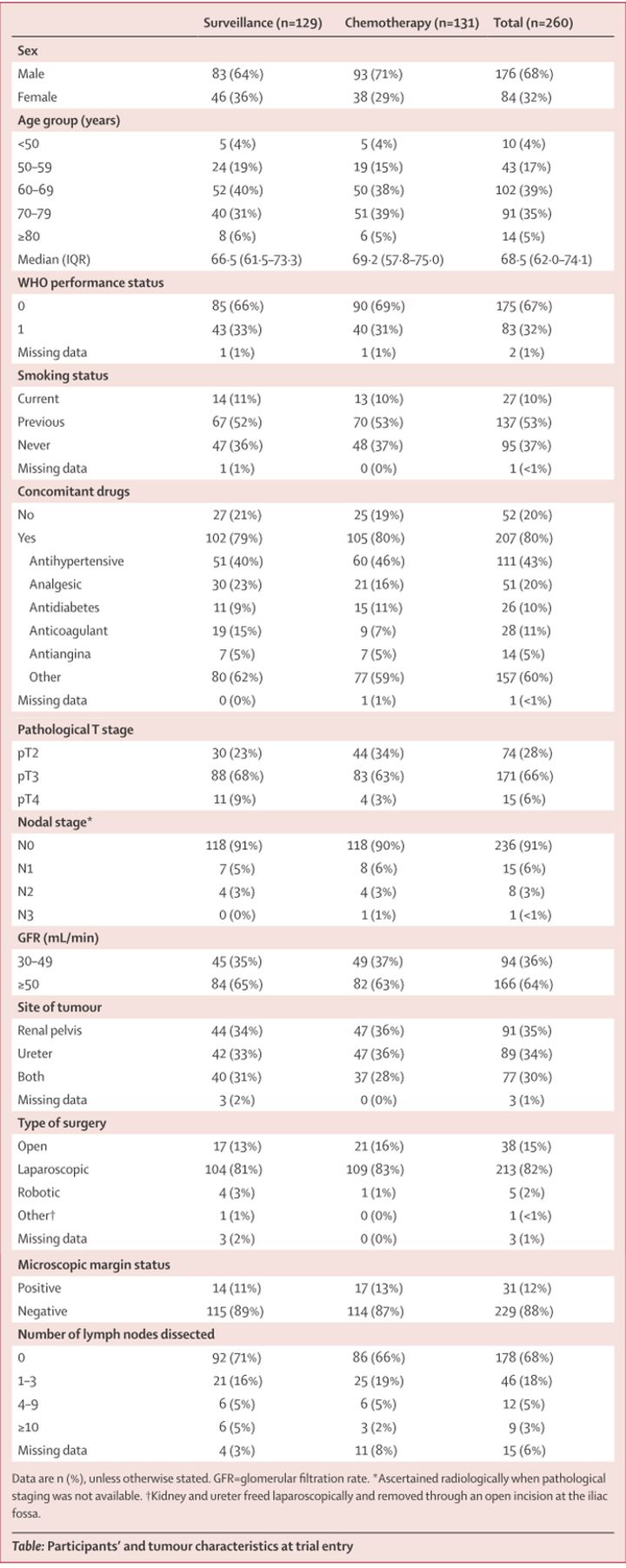
在POUT中,从2012年6月19日至2017年11月8日,研究人员选择在英国71家医院中招募接受根治性肾输尿管切除术,且术后分期为T2-T4 N0-N3 M0或者任意T 分期N1-3 M0的UTUC患者,进行开放标签的随机对照III期试验。研究采用最小化随机算法将招募的261名患者按1:1随机分配入对照组(n=129)或者吉西他滨-顺铂(吉西他滨-卡铂,如果GFR为30-49ml / min)辅助化疗组(n=132,接受4个21天化疗周期)。
用药方案为:患者需要在手术后90天内开始化疗;第1天静脉注射顺铂(剂量为70mg /m²)或者卡铂[剂量为曲线下面积(AUC)4.5/5,并且仅对于肾小球滤过率(eGFR)低于50mL/min],以及在第1天和第8天静脉给予吉西他滨(剂量为1000mg/m²)。
患者接受6个月的影像学检查和2年的膀胱镜检查,然后每年5年。主要终点为无病生存期,次要终点为无转移生存期,总体生存期,毒性和患者报告的生活质量。由于有效性的证据,该试验已在独立数据监测委员会的建议下提早结束招募。 POUT的试用方案如下:
从2012年5月到2017年11月,在英国的56个中心招募了261名患者(129例监测; 132例化学疗法)。 这些患者的中位年龄为69岁(范围37-88),pT2为28%,pT3为66%,pN0为91%。
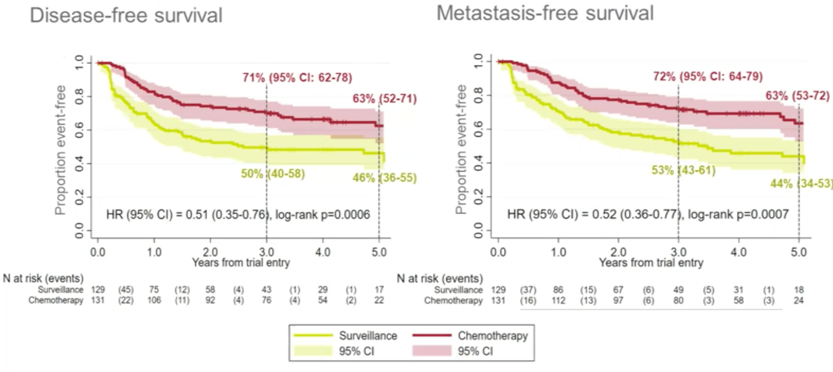
在48.1个月的中位随访期(IQR:36.0-60.1)中,无病生存的未经调整风险比为0.51(95%CI 0.35-0.76; p = 0.0006),无转移生存为0.52(95%CI) 0.36-0.77; p = 0.0007)
在随访期间,有93/260(35.8%)例患者死亡(监视率为52/129 [40.3%],化疗为41/131 [31.3%])。 化学疗法使相对死亡风险降低了30%(但统计学上无统计学意义)(HR 0.70,95%CI 0.46-1.06; p = 0.09)
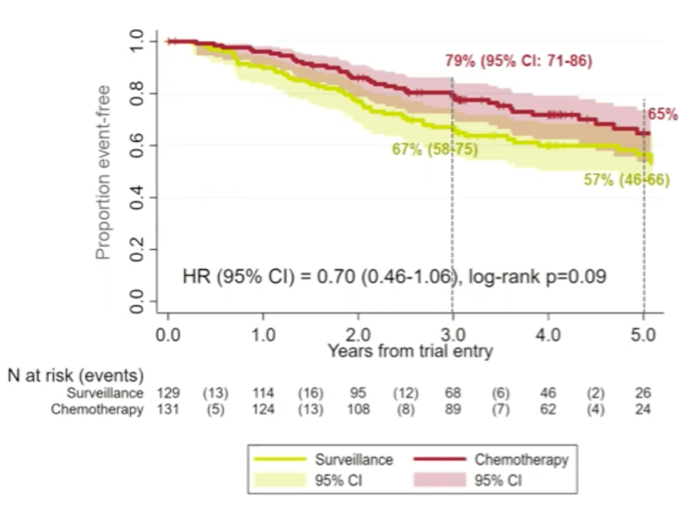
监测患者的3年总生存率为67%(95%CI 58-75%)和化疗的79%(95%CI 71%-86%)。 没有证据表明与化疗相关的长期毒性,最常见的2级以上不良反应为高血压(10.4%),嗜睡(10.4%)和听力下降(5.4%)。 没有证据表明治疗后12个月的生活质量有统计学上或临床上的相关差异(EORTC Q30全球健康状况在12个月和24个月分别为4.1和4.8的平均差异,赞成化疗)。
Birtle博士总结了对POUT III期临床试验的最新分析,得出以下结论:
通过额外的随访,维持了辅助化疗对无病生存和无转移生存的益处。
总体生存率有非统计学显着性改善
这些最新分析支持使用铂类辅助化疗作为推荐的护理标准
原始出处:
Birtle A, Johnson M, Chester J, et al. Adjuvant chemotherapy in upper tract urothelial carcinoma (the POUT trial): a phase 3, open-label, randomised controlled trial. Lancet (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#上尿路尿路上皮癌#
41
#III#
33
#ASC#
36
#上皮癌#
35
#III期#
24