Cancers:水溶性SIGLEC5 (sSIGLEC5):结直肠癌的新预后指标
2021-08-03 yd2015 MedSci原创
该研究表明,水溶性SIGLEC5 (sSIGLEC5)是结直肠癌患者的预后指标。
结直肠癌(CRC)是全球常见的消化道恶性肿瘤。左右半结直肠癌的临床特征、预后以及对治疗的反应均有差别。因此,左右半结直肠癌被认为是两种疾病,也说明了结直肠癌是一种异质性较强的疾病。CEA一直是被用于结直肠癌的辅助诊断,疗效检测,但是其特异性不强,很多肿瘤也都有不同程度的升高。因此,寻找有效的预后指标也是迫切需要的。发表在Cancers杂志上的研究表明,水溶性SIGLEC5 (sSIGLEC5)是结直肠癌新的预后指标。
2015年5月28日至2020年8月11日,共有114名CRC患者以及67例健康人群纳入研究。CRC患者术前24小时采集血样,并且随访至2021年4月7日。CRC患者按照肿瘤分期(I、II、III、IV期)进行分析。
对比健康人群,CRC患者血浆中的sSIGLEC5水平明显升高,有统计学差异(p ≤ 0.0001),而且在死亡患者中sSIGLEC5的水平也是明显高于生存者的。
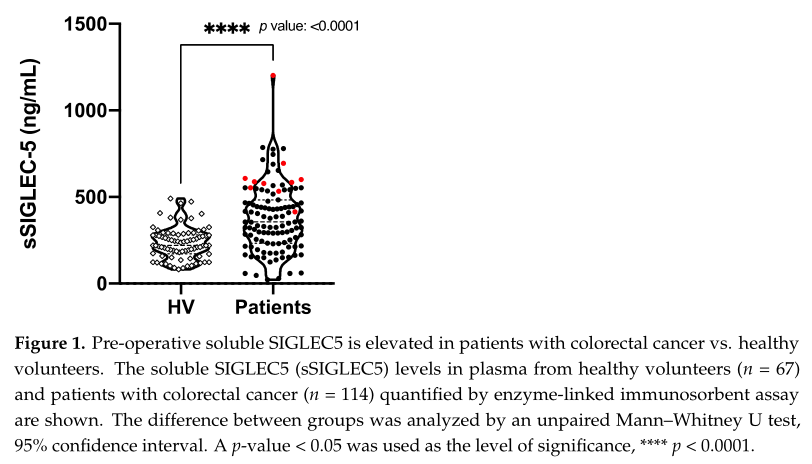
CRC和健康人群的水平比较
接着分析不同分期患者中的sSIGLEC5水平,可以发现随着分期增加,sSIGLEC5水平越高,并且与患者的分期成正向相关(Pearson r = 0.2595, p = 0.005)。类似的,sSIGLEC5水平与患者的分级、淋巴结侵犯等相关。

不同分期和相关性分析
为区分死亡和生存患者,研究者进行ROC曲线分析,AUC为0.853; 95% CI 0.7729–0.9344; 有统计学差异(p = 0.0001)。而最佳分解值为412.6 ng/mL,表现出现较高的敏感性(1; 95% CI 74.12–100) 和特异性(0.67,95% CI 57.31–75.44)。
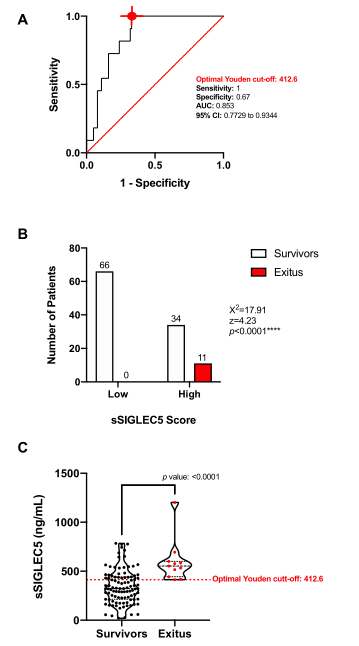
ROC
Wald回归模型分析以下变量是否是独立预后因素: 年龄、性别、分期、治疗方式、肿瘤大小、淋巴结转移、淋巴管侵犯、神经侵犯、手术切缘、CEA、分级和sSIGLEC5。研究发现只有分级和sSIGLEC5是独立的预后因素。
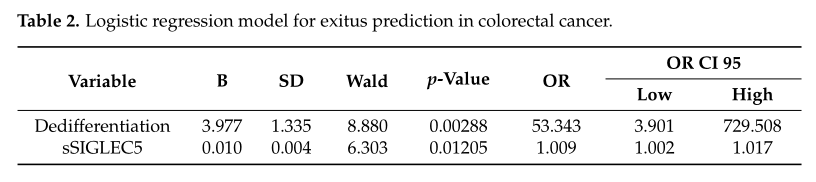
回归分析预后因素
Kaplan–Meier 曲线进行生存分析,高水平sSIGLEC5 患者较低水平患者的总生存(OS)明显缩短(HR=15.68; 95% CI 4.571–53.81; p ≤ 0.0001)。
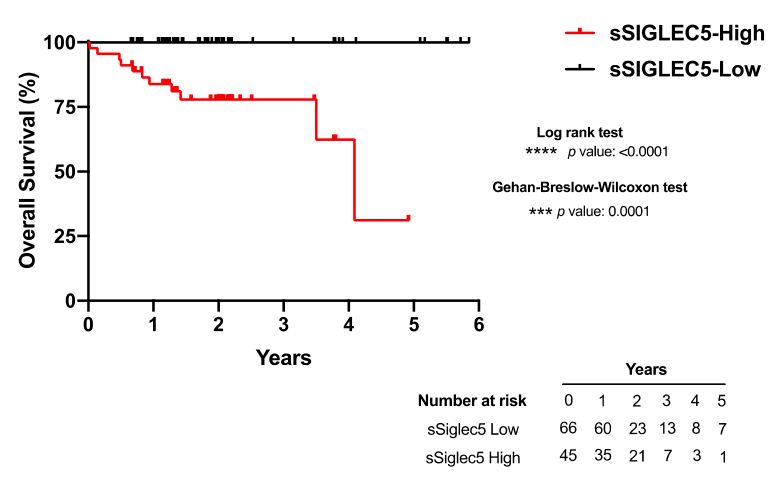
生存分析
综上,该研究表明,水溶性SIGLEC5 (sSIGLEC5)是结直肠癌患者的预后指标。
原始出处:
Montalbán-Hernández, K.;Cantero-Cid, R.; Lozano-Rodríguez, R.; et al. Soluble SIGLEC5: A New Prognosis Marker in Colorectal Cancer Patients. Cancers 2021, 13, 3896. https://doi.org/10.3390/cancers13153896.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#SSI#
44
#ERS#
46
#预后指标#
53
#结直肠#
40
学习啦~
70