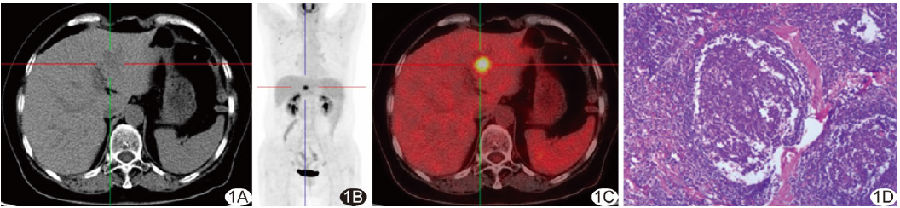
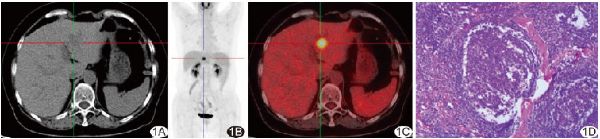
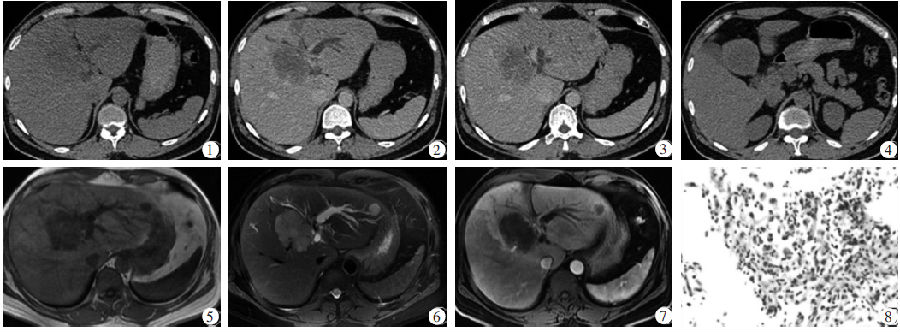
肝脏局灶型巨淋巴结增生症的18F-FDG PET/CT表现1例
2018-10-19 麻广宇 徐白萱 关志伟 中国医学影像技术
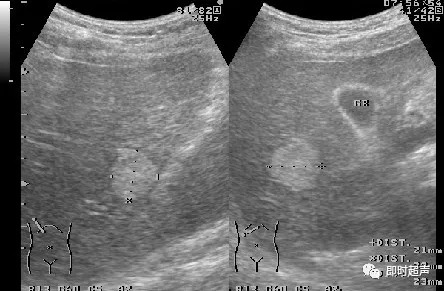
患者女,63岁。因体检超声发现肝占位1月余入院。患者无发热、恶心、呕吐、腹部疼痛及后背放射痛。既往有结核病史,已治愈;8年前因子宫息肉接受子宫切除术。实验室检查:淋巴细胞比例升高(0.401),白细胞计数增高(107.7×109/L),乙型病毒性肝炎阴性,肿瘤标志物血清癌胚抗原、甲胎蛋白及CA19-9均正常。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










单发肝内和单侧肾脏的CD极为罕见,一般好发肺门纵隔,山西肿瘤山西大医院至今都无法确诊我妈此病,只要体温控制好,壳寡糖确认有媲美抗生素的消炎抗炎效果,准备订购蜂胶滴液继续口服。暑期降温只能燕窝不间断,体温升高是恶化征象之一。
64
#巨淋巴结增生症#
38
#8F-FDG#
37
#PE#
30
#淋巴结#
33
#PET/CT#
45
#PET#
26
#CT表现#
38
学习了
56