Nat Commun:转录组学分析揭示FGF1对2型糖尿病的缓解作用
2020-09-15 QQY MedSci原创
2型糖尿病(T2D)是当前社会面临的最常见且最昂贵的生物医学挑战之一。该疾病的标准治疗涉及每天服用一种或多种抗糖尿病药物,虽具有一定的疗效,但仍无法为大多数患者提供足够的血糖控制。因此,探究更有效的治
2型糖尿病(T2D)是当前社会面临的最常见且最昂贵的生物医学挑战之一。该疾病的标准治疗涉及每天服用一种或多种抗糖尿病药物,虽具有一定的疗效,但仍无法为大多数患者提供足够的血糖控制。因此,探究更有效的治疗策略迫在眉睫。
近期研究显示,在Lepob/ob小鼠和其他T2D啮齿动物模型中,单次脑室内(intracerebroventricular,icv)注射FGF1(成纤维细胞生长因子1)可以实现糖尿病的持续性缓解,内侧基底下丘脑(MBH)被确认为负责该效应的大脑区域。
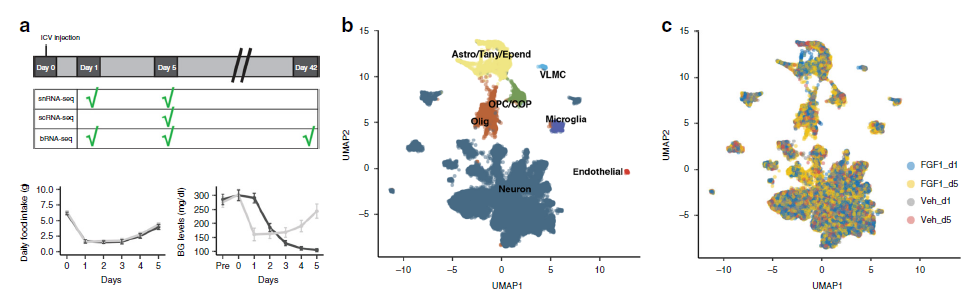
脑室内注射FGF1研究设计及诱导的细胞应答反应
单细胞RNA测序(scRNA-seq)作为测量下丘脑中单细胞的基因表达的一种有效的技术。为了更好地了解MBH中细胞对FGF1的应答反应,研究人员在脑室内注射FGF1或对照的第1天和第5天,对来自糖尿病Lepob/ob小鼠下丘脑的> 79,000个单细胞转录组进行了测序。
研究人员在多种类型的下丘脑细胞中均观察到对FGF1的广泛转录应答,而在这两个时间点里,神经胶质类细胞表现出比神经元更强的应答水平。
脑室内注射FGF1对Agrp神经元的影响
在注射第1天,单核细胞和室管膜细胞是FGF1应答最强的细胞类型,而随后星形胶质细胞和少突胶质细胞表现出最强应答水平。组化实验和超微结构证实星形胶质细胞和Agrp神经元(下丘脑黑皮质素系统的关键组成成分)之间的细胞间相互作用增强,进一步的研究显示,完整的黑皮质素信号对于FGF1的持续抗糖尿病作用是必不可少的。
综上研究结果显示,下丘脑神经胶质细胞是FGF1作用的主要靶标,而持续性的糖尿病缓解作用依赖于完整的黑皮质素信号。
原始出处:
Bentsen, M.A., Rausch, D.M., Mirzadeh, Z. et al. Transcriptomic analysis links diverse hypothalamic cell types to fibroblast growth factor 1-induced sustained diabetes remission. Nat Commun 11, 4458 (07 September 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
32
#COMMUN#
37
#转录#
31
#FGF1#
38
#转录组#
32
学习
70
谢谢MedSci提供最新的资讯
42