J Clin Oncol:新型二代CD19-CAR T细胞治疗复发/难治性B-ALL成人患者的效果和安全性
2021-09-01 Nebula MedSci原创
一种新型的二代 CD19-CAR(CAT19-41BB-Z),具有快速关闭率,专为更多生理性 T 细胞活化而设计,可降低毒性并改善植入效果
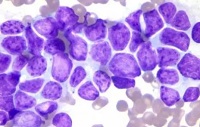
成人 B 细胞急性淋巴细胞白血病 (B-ALL) 的预后很差。目前尚没有获批治疗该病的 CD19 嵌合抗原受体 (CAR) 疗法。Roddie等研究人员开发了一种新型的二代 CD19-CAR(CAT19-41BB-Z),具有快速关闭率,专为更多生理性 T 细胞活化而设计,以降低毒性并改善植入效果。
多中心的 1 期 ALLCAR19 试验评估了自体 CAT19-41BB-Z CAR T 细胞(AUTO1)用于复发性或难治性(r/r)成人 B-ALL 患者的安全性和初步疗效。
该试验招募了年满 16 岁的 r/r B-ALL 患者。主要终点是毒性和 CAR T细胞的制备可行性。次要终点是第 1 和第 3 个月时的缓解深度、CAR-T 细胞持续时间、低丙种球蛋白血症和 B 细胞发育不全的发生率和持续时间,以及第 1 年和 第 2 年时的无事件生存期和总生存期。
25 位患者接受了白细胞清除术,成功制备了 24 位患者的 CAR T细胞,最终 20 位患者输注了 AUTO1。受试患者中位年龄为 41.5 岁,25%的既往采用过博纳吐单抗治疗、50%的既往接受过伊妥珠单抗奥佐米星治疗、65%的既往进行过异体干细胞移植。在预处理时,45% 的患者骨髓原始细胞≥ 50%。
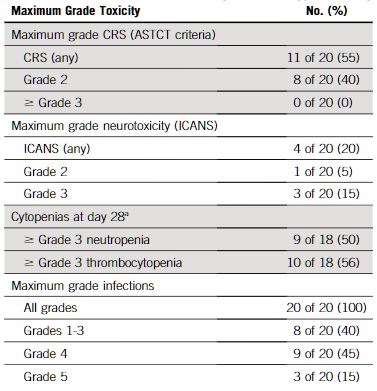
不良反应事件
没有患者出现≥ 3 级的细胞因子释放综合征。20 位患者中的 3 位 (15%) 发生了 3 级神经毒性,在使用类固醇 72 小时内减轻至 ≤ 1 级。17 位(85%)患者在第 1 个月时达到了微小残留病灶阴性(完全缓解),其中 3 位在缓解期间进型了同种异体干细胞移植。
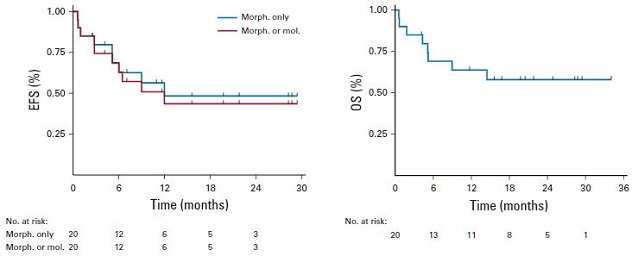
无进展生存期和总生存期
第 6 个月和第 12个月时的无事件生存率分别为68.3%(95%CI 42.4-84.4)和48.3(23.1-69.7)。在最后一次随访时,20 位患者中有 15 位持续存在 B 细胞再生障碍,观察到高水平扩增(Cmax 127152 拷贝/μg 基因组 DNA)和持久的 CAR-T 持久性。
综上所述,在 r/r 成人 B-ALL 患者中,AUTO1 表现出可耐受的安全性、高缓解率和优秀的持续时间。该研究结果支持进一步将 AUTO1作为 r/r 成人B-ALL 的发展计划。
原始出处:
Claire Roddie, et al. Durable Responses and Low Toxicity After Fast Off-Rate CD19 Chimeric Antigen Receptor-T Therapy in Adults With Relapsed or Refractory B-Cell Acute Lymphoblastic Leukemia. Journal of Clinical Oncology. August 31, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.00917
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
33
#ALL#
34
#CD19#
40
#B-ALL#
41
#难治性#
29
谢谢梅斯分享这么多精彩信息
54
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
51
好文章,谢谢分享。
0