Clin Cancer Res:二代紫杉烷卡巴他赛治疗转移性胃癌的疗效
2020-09-17 MedSci原创 MedSci原创
本研究是一项多中心的II期临床试验,旨在研究一种新型二代紫杉类药物卡巴他赛(cabazitaxel)治疗转移性胃癌的疗效和安全性。
受试患者为经一线或多线治疗后进展的局部晚期、不能手术切除的或转移性胃癌患者,既往是否采用过紫杉烷类药物治疗都可以,将用或没用过紫杉烷治疗的患者进行独立疗效评估。主要终点是无进展存活期(PFS)。同时本研究还进行了全外显子和肿瘤RNA测序。

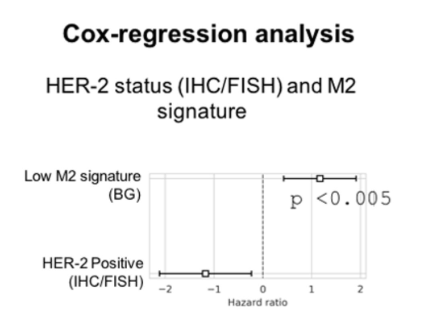
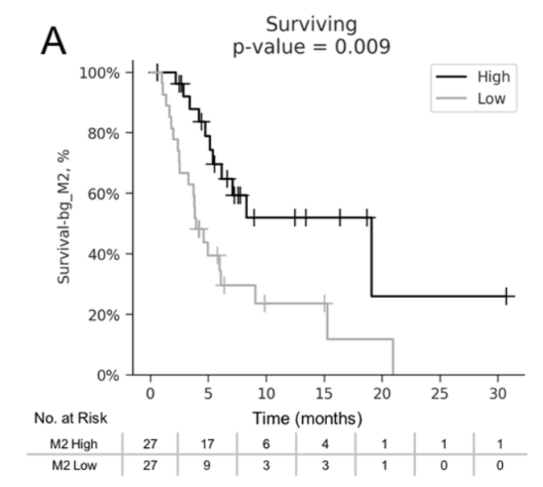
终上所述,卡巴他赛在晚期胃癌中有适度的活性,包括既往使用紫杉类药物治疗的患者。HER2扩增/过表达和M2高巨噬细胞标记是紫杉烷疗效的潜在生物标志物,值得进一步评估。
原始出处:
Manish A. Sha, et al. Multicenter Phase II Study of Cabazitaxel in Advanced Gastroesophageal Cancer: Association of HER2 Expression and M2-Like Tumor-Associated Macrophages with Patient Outcome. Clin Cancer Res. September 15 2020 26 (18) 4756-4766; DOI:10.1158/1078-0432.CCR-19-3920
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#转移性胃癌#
45
#紫杉烷#
38
#转移性#
42
#卡巴他赛#是新一代紫杉类药物,Cabazitaxel的抗癌作用机制和特点与多西他赛相似,属于抗微管类药物。卡巴他赛通过与微管蛋白结合,促进其组装成微管,同时可阻止这些已组装好了的微管**,使微管稳定,进而抑制细胞的有丝分裂,和间期细胞功能(interphase cellular functions)的发挥。与第一代多西他赛相比,作用可能更好,这是很难得化疗药物的进一步发展,在晚期#胃癌#中有适度的活性
239
谢谢梅斯提供这么好的信息,学到很多
0
#卡巴他赛#
159
不错不错
92
学习
85
学习
81
进来学习下
36