EU :腹腔镜 VS 机器人 哪种方式进行根治性前列腺切除术更好?
2021-08-17 泌尿小王 MedSci原创
根治性前列腺切除术(RP)后尿失禁深深地影响患者生活质量。机器人辅助根治性前列腺切除术(RARP)和腹腔镜RP (LRP)是常用的手术方式,研究显示它们对肿瘤治疗效果无差异,而前者对控尿更好。
根治性前列腺切除术(RP)后一过性或持续性尿失禁深深地影响患者生活质量。目前,机器人辅助根治性前列腺切除术(RARP)由于其放大的视野和高精度,被认为可以提供最佳的肿瘤和功能结果腹腔镜RP (LRP)和RARP哪种方式对患者效果更好仍然缺乏相关研究。
最近,《欧洲泌尿外科杂志》(EU)发表了一项研究结果显示:LRP与RAPR对肿瘤治疗效果没有差异,但是就术后三个月尿控而言,后者更好一些。
临床设计
手术人员要求
(1)所有外科医生均有RARP和LRP的经验,每一种类型的手术超过150例。
(2)因为大多数德国患者更喜欢在机器人的帮助下进行手术,参与者以3:1的比例被随机分配进行RARP或LRP。
(3)在3个月的评估和初步研究结果的提取结束之前,患者对手术方法进行盲法。一旦患者被告知所进行的手术类型,在开放试验的背景下获得患者报告的6个月和12个月的结果。
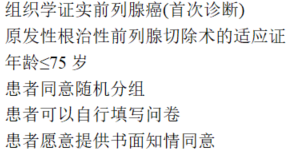
纳入标准
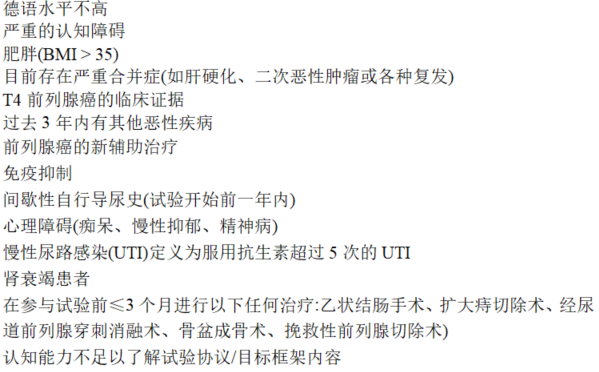
排除标准
手术方式
(1)根据医生的选择,采用经腹膜或腹膜外入路,并根据D ‘Amico标准对所有中、高危患者进行盆腔淋巴结清扫(PLND)。
(2)所有淋巴结清扫均使用标准化的扩展PLND模板,上缘为髂总动脉。
注:术前神经保留是根据临床标准设计的,在手术过程中根据冰冻切片方案进行修改(有证据表明束侵犯后,在患侧进一步切除束)。根据外科医生的决定和局部术后协议,患者在取出引流管后出院。所有患者均接受盆底训练指导。
随访安排
患者在入院时、术后1、3、6和12个月评估功能和肿瘤预后,同时在24和36个月收集长期肿瘤预后(前列腺特异性抗原)
研究的主要指标
(1)拔除尿管后三个月尿失禁恢复情况。(24h内未使用尿垫则认为恢复正常)。
次要指标
(1)术后1,3, 6,12月进行以下的问卷评估
(2)失禁问卷简表咨询(ICIQ-SF)
(3)国际勃起功能指数(IIEF-5)
(3)欧洲癌症研究与治疗组织生活质量调查问卷(EORTC-QLQ)
(4)医院焦虑和抑郁量表(HADS-D)
(5)肿瘤结果定义为术后3、6、12、24和36个月的手术边缘阳性和生化复发。
结果
总共纳入患者782 人
主要指标
(1)在随访3个月时,54%的RARP患者没有使用衬垫或安全衬垫,LRP患者的比例为46%
次要指标
(2)在双侧神经保留的患者中,机器人辅助的优势更为明显,66%的RARP患者处于稳定控尿状态,而50%的LRP患者处于稳定控尿状态。
(3)绝大多数失禁患者报告每天都有少量尿漏,只有9.3%的RARP患者和15%的LRP患者报告中度至大量尿漏。
(4)根据ICIQ-SF,RARP和LRP对术后患者1个月 和3个月尿失禁的主观评价也有统计学差异 。
(5)EORTCPR-25评估的生活质量在机器人辅助下也得到了更好的保存。
进一步分析的结果
(1)双侧神经保留患者的控尿比例差异更大(RARP: 66%, LRP:49%;p = 0.005)。
(2)年龄>65岁和不保留神经手术不利于控尿:
(3)年龄>65岁控尿的HR = 0.69 (0.54-0.86,p = 0.001);
(4)不保留神经控尿的HR = 0.56 (0.43-0.72, p <0.0001);
(5)单侧神经保护(vs双侧神经保护)HR = 0.66 (0.44 0.98),p = 0.038。
ICIQ-SF评分也反映出,与LRP组患者相比,RARP组患者在3个月时的禁尿结果有改善。
肿瘤治疗效果
RARP和LRP在早期肿瘤预后方面没有显著差异。
这两种技术都显示比较了阳性边缘的手术效果(19% for RARP and 14% for LRP; p = 0.19) 淋巴结浸润率(RARP为7.8%,LRP为4.8%;p = 0.38
性功能方面
(1)在术后3个月,分别有18%和6.7%的接受神经保留(双侧或单侧)RARP和LRP的患者报告勃起足以性交(p = 0.007)。
(2)LRP组的IIEF总和平均比RARP组的IIEF总和降低了1.54分(p = 0.026)。
(3)然而,EORC-PR25调查问卷显示,在3个月时,两种技术在性功能和性活动方面没有显著差异。
(4)保留双侧和单侧神经增强了勃起功能恢复,年龄与性功能恢复呈负相关(2.53)。然而,使用的各种工具对效力恢复的评估并不一致。
并发症
LRP组患者的并发症发生率较高,但是没有差异(Clavien-Dindo分级):RARP组87例(15%),LRP组41例(21%)发生任何级别的并发症(p = 0.097)。
结论
与腹腔镜入路相比,RARP术后3个月早期失禁恢复较好。年龄和术中神经保留技术进一步影响失禁恢复。在机器人辅助下勃起功能恢复也得到改善,但围手术期发病率和早期肿瘤预后无明显差异。
参考文献
Stolzenburg J-U, et al. Robotic-assisted Versus Laparoscopic Surgery: Outcomes from the First Multicentre, Randomised, Patient-blinded Controlled Trial in Radical Prostatectomy (LAP-01). Eur Urol (2021), https://doi.org/10.1016/j.eururo.2021.01.030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前列腺切除#
48
#切除术#
34
#腹腔镜#
39
#机器人#
42
#机器#
48
#根治#
28