AGING CELL:表观年龄是移植人造血细胞的内在特性
2019-02-10 海北 MedSci原创
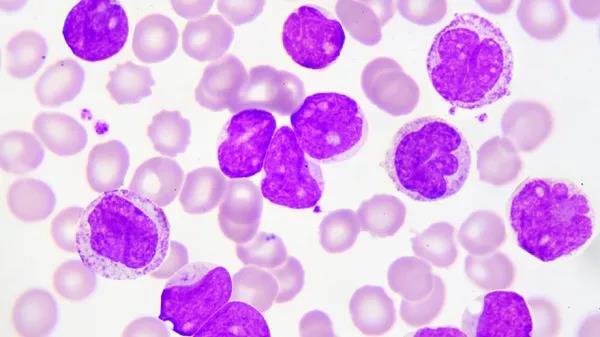
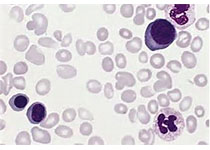
最近,基于短期观察的研究表明,异基因造血干细胞移植(HSCT)后重建血液的DNAm年龄反映了供体的年龄。然而,至今为止,尚不清楚供体血液的DNAm年龄是否长期与受体的年龄无关。
通过DNA甲基化分析可以准确估计组织和细胞的年龄。多组织DNA甲基化(DNAm)年龄预测因子结合了353个CpG二核苷酸的DNAm水平,以达到称为DNAm年龄的年龄估计。
最近,基于短期观察的研究表明,异基因造血干细胞移植(HSCT)后重建血液的DNAm年龄反映了供体的年龄。然而,至今为止,尚不清楚供体血液的DNAm年龄是否长期与受体的年龄无关。重要的是,包括儿童接受者在内的长期研究有可能清楚地揭示DNAm年龄是细胞内在特质,还是由细胞外因子所调节的。
最近,研究人员通过分析HSCT供体和受体对的血液甲基化数据来解决这个问题,这些供体和受体对在实际年龄上(年龄差异在1到49岁之间)差异很大。
研究人员发现重建血液的DNAm年龄不受受体年龄的影响,即使是HSCT后17年内没有血液系统疾病复发的个体中也是一样。然而,白血病复发的受体DNAm年龄不稳定。
这些数据与研究人员之前关于癌细胞DNAm异常年龄的研究结果一致,可以利用它来监测HSCT受体的健康状况。
因此,该数据表明,移植的人造血干细胞具有内在的DNAm年龄,不受不同年龄的受体环境的影响。
原始出处:
Arne Søraas et al. Epigenetic age is a cell‐intrinsic property in transplanted human hematopoietic cells. Aging Cell, 2019; doi: https://doi.org/10.1111/acel.12897
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
29
#人造#
32
#CEL#
25
#血细胞#
33
#造血#
27
#造血细胞#
30
很好的学习机会
46
学习了,谢谢作者分享!
43