CLIN CANCER RES:循环肿瘤DNA出现RAS紧急突变对帕尼单抗治疗转移性结直肠癌的影响
2018-11-22 MedSci MedSci原创
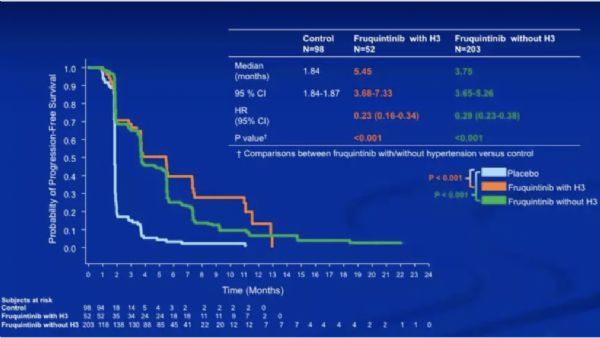
抗EGFR治疗期间出现RAS突变可能是获得抗EGFR治疗耐药的机制,从而引起人们关注。循环肿瘤(ct)DNA检测是一种确定RAS突变状态的微创且高敏感的方法。CLIN CANCER RES近期发表了一篇文章,研究治疗期间循环肿瘤DNA出现RAS紧急突变对转移性结直肠癌治疗耐药的影响。
抗EGFR治疗期间出现RAS突变可能是获得抗EGFR治疗耐药的机制,从而引起人们关注。循环肿瘤(ct)DNA检测是一种确定RAS突变状态的微创且高敏感的方法。CLIN CANCER RES近期发表了一篇文章,研究治疗期间循环肿瘤DNA出现RAS紧急突变对转移性结直肠癌治疗耐药的影响。
作者通过二代测序技术检测接受帕尼单抗治疗患者中RAS ctDNA突变情况。在基线和治疗后收集血浆样品检测RAS突变是否存在。研究结果表明,接受panitumumab治疗的患者(n = 238)在基线时有188例(79%)是野生型(WT)RAS,50例(21%)是突变RAS。基线ctDNA WT RAS的188名患者中,164名患者可评估治疗后结果,其中有32%的患者出现RAS紧急突变。基线时ctDNA 判断的WT和RAS突变状态的患者中位总生存分别为13.7和7.9个月。ctDNA 是否出现紧急RAS突变的患者临床结局没有显着差异。
原始出处:
Tae Won Kim, Marc Peeters, et al. Impact of Emergent Circulating Tumor DNA RAS Mutation in Panitumumab-Treated Chemoresistant Metastatic Colorectal Cancer. CLIN CANCER RES. November 2018 doi: 10.1158/1078-0432.CCR-17-3377
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#转移性#
0
#帕尼单抗#
35
#结直肠#
28
#循环肿瘤DNA#
32
#紧急#
32
了解一下谢谢
0
了解一下,谢谢分享!
67