Acta Neuropathologica: 评估死后大脑路易病理学的神经病理学共识标准: 一项多中心研究
2021-01-06 MedSci原创 MedSci原创
路易体病(LBD)包括帕金森病(PD)、轻度认知障碍性帕金森病(PD-MCI)、痴呆性帕金森病(PDD)和路易体痴呆症(DLB),这些疾病都有特征性的临床表现和相关的临床诊断标准。
路易体病(LBD)包括帕金森病(PD)、轻度认知障碍性帕金森病(PD-MCI)、痴呆性帕金森病(PDD)和路易体痴呆症(DLB),这些疾病都有特征性的临床表现和相关的临床诊断标准。这些临床症状的神经病理学特征是Lewy病理学(LP),它包括神经细胞体和神经细胞中的α-突触核蛋白聚集体过程:路易体(LB)和Lewy神经突(LN)。然而,LP也可见于缺乏明显临床症状的个体。偶发性LBD一词最初是为缺乏帕金森病或认知症状但局限于脑干的LP而创造的,但最近,它被扩展到包括杏仁核为主和仅嗅觉的LP。
目前,路易体病(LBD)的神经病理学诊断可根据几个分期系统进行,包括Braak-Lewy体分期(Braak)、McKeith及其同事的共识标准(McKeith)、Leverenz及其同事的改良McKeith系统(Leverenz),以及Beach及其同事(Beach)的统一分期系统。所有这些系统在确定的皮质和皮质下区域使用路易病理学(LP,即路易体和路易神经突起)的半定量评分(4或5级量表)。
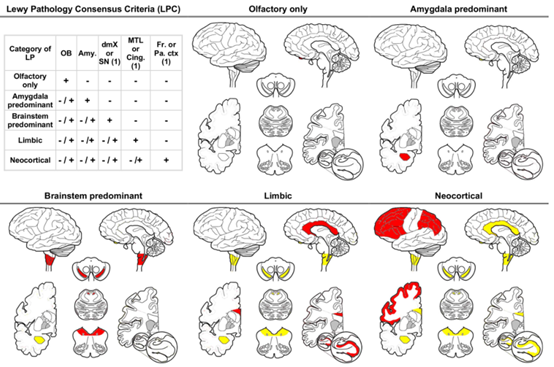
虽然这些系统被广泛使用,但有些系统的可靠性较低和/或无法明确地用LP对所有病例进行分类。为了解决这些局限性,我们设计了一个新的系统,LP一致性标准(LPC),它是基于McKeith系统,但适用于LP评分的二分法并包括杏仁核为主和仅嗅觉阶段。
本研究主要由16名评分员根据Braak,McKeith,Leverenz、Beach和LPC系统对34例LP患者的脑干、边缘系统、新皮质和嗅球的α-突触核蛋白染色切片进行扫描和评估。McKeith、Leverenz和LPC系统能达到良好水平(Krippendorff的α≈0.6),而Braak和Beach系统的评分者间信度分别较低(Krippendorff的α≈0.4)。使用LPC系统,大多数评分员都能明确地对所有病例进行分类,当使用Beach系统时,这一比例为97.1%。然而,当使用Leverenz(11.8%)、McKeith(26.5%)或Braak(29.4%)系统时,相当一部分病例无法分类。
综上所述,LPC系统具有良好的可重复性,并允许将所有案例分类为不同的类别,有希望成为未来LP基本尸检评估的标准方法。
Attems, J., Toledo, J.B., Walker, L. et al. Neuropathological consensus criteria for the evaluation of Lewy pathology in post-mortem brains: a multi-centre study. Acta Neuropathol (2021). https://doi.org/10.1007/s00401-020-02255-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#pathologic#
48
#多中心研究#
50
#CTA#
43
#Pathol#
46
#多中心#
42
#病理学#
57
#神经病#
39
#神经病理#
42