Neurology:牵牛花视盘发育异常
2018-11-07 zyx整理 神经科病例撷英拾粹
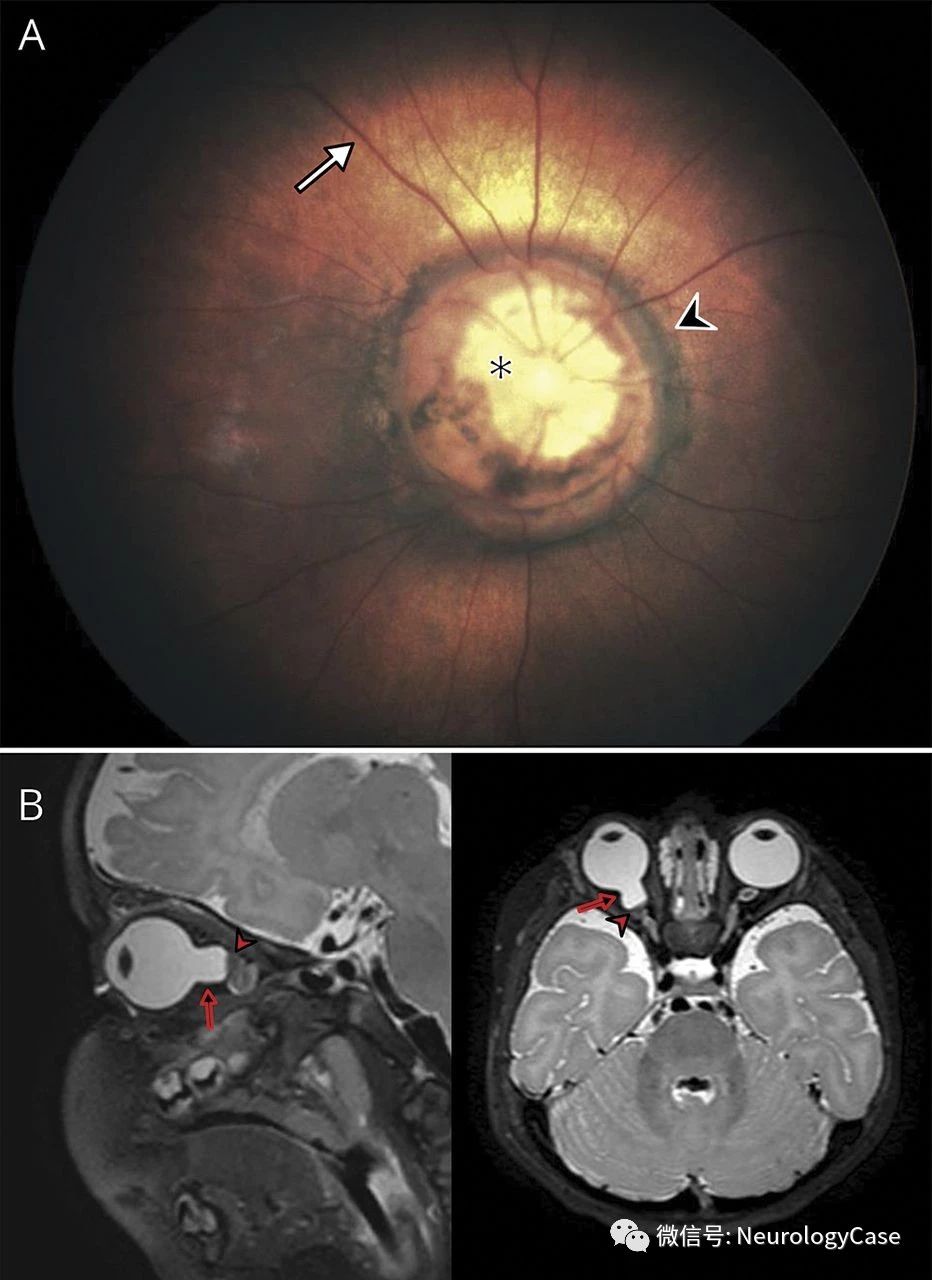
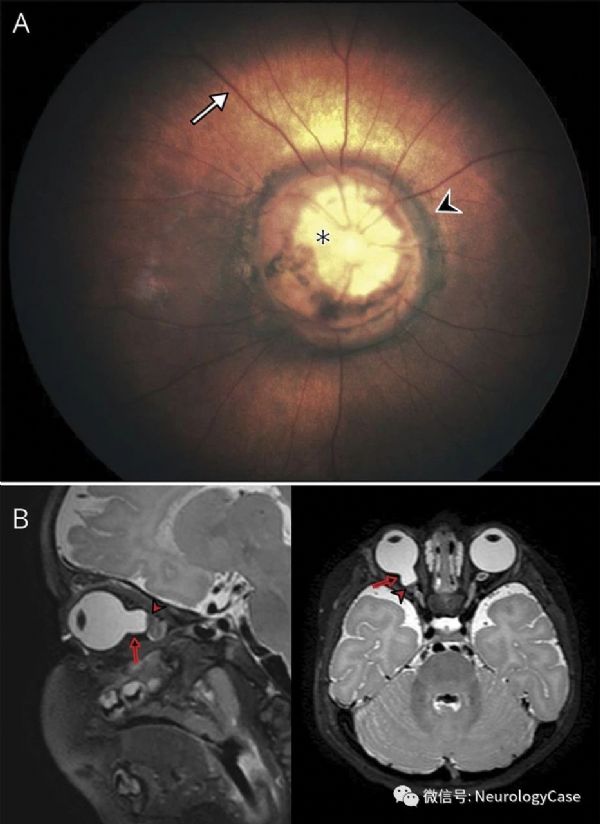
7个月大女婴,表现为斜视。眼底镜检查(图A)提示右眼典型的牵牛花视盘发育异常(morning glory disc anomaly,MGDA),包括视神经盘扩大的漏斗样凹陷,视乳头周围色素环和视网膜血管辐射状分布。
7个月大女婴,表现为斜视。眼底镜检查(图A)提示右眼典型的牵牛花视盘发育异常(morning glory disc anomaly,MGDA),包括视神经盘扩大的漏斗样凹陷,视乳头周围色素环和视网膜血管辐射状分布。脑MRI(图B)显示视神经附着处凹陷伴异常组织,符合胶质簇。由MGDA引起的症状是多种多样的且并不总是存在:受累眼睛视敏度异常(通常较差),视野缺损和盲点扩大是最常见的症状。可出现浆液性视网膜脱落。通常为单侧。MRI有助于诊断和发现相关的颅内异常,特别是中线部位发育异常,如经蝶窦基底脑膨出和moyamoya综合征。MGDA没有理想的治疗方法;然而,提升视力对于预防弱视非常重要。
(图:A:右眼眼底检查可见视盘[*]漏斗状凹陷,视乳头周围区域[箭头]的色素环以及视网膜血管辐射状分布[箭头];B:T2WI可见视神经附着处凹陷[箭]和胶质簇形成[箭头])
原始出处:Poillon G, Gillard P, Lecler A. Teaching NeuroImages: Morning glory disc anomaly. Neurology. 2018 Oct 9;91(15):e1457-e1458.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#发育异常#
31
#Neurol#
34
#发育#
33