Nat Commun:研究定义了PD-L1阴性ER阳性乳腺癌患者的新型免疫特征
2020-10-06 MedSci原创 MedSci原创
在雌激素受体(ER)阳性乳腺癌中,对免疫治疗的反应并不常见,并且迄今为止缺乏预测性标志物。
在雌激素受体(ER)阳性乳腺癌中,对免疫治疗的反应并不常见,并且迄今为止缺乏预测性标志物。

这项随机II期研究将检查点抑制剂治疗ER阳性乳腺癌患者的表观遗传学引物的安全性和反应率定义为主要终点。次要和探索性终点包括PD-L1调控和T细胞免疫信号。
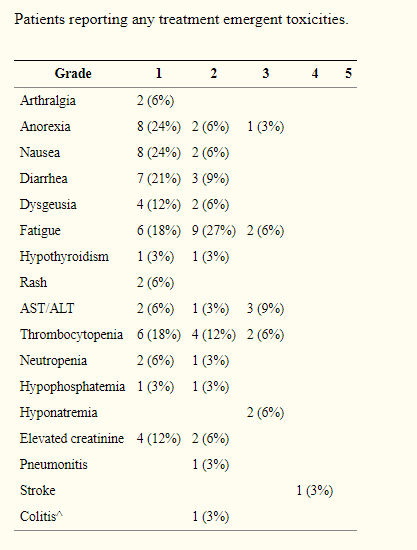
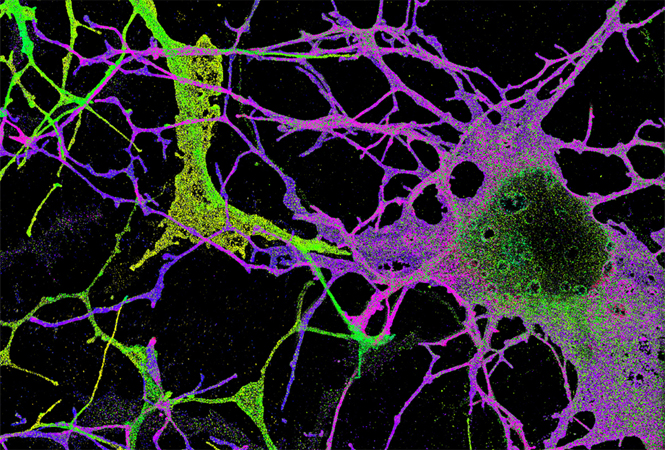
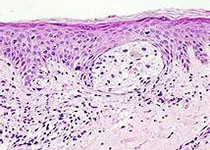
结果,34名患者接受了伏立诺他、他莫昔芬和pembrolizumab,在之前的五种转移治疗方案进展后无过度毒性。客观反应为4%,临床获益率(CR+PR+SD>6 m)为19%。在5/5的临床获益患者的肿瘤或血液中可见T细胞衰竭(CD8+ PD-1+/CTLA-4+)和治疗调节性T细胞衰竭(CD4+ Foxp3+/CTLA-4+),但只有1例无反应者。肿瘤淋巴细胞浸润率为0.17%。只有两名无反应者的PD-L1表达量大于1%。
综上所述,该数据定义了PD-L1阴性ER阳性乳腺癌患者的新型免疫特征,这些患者更可能从免疫检查点和组蛋白去乙酰化酶抑制中获益。
原始出处:
Manuela Terranova-Barberio, Nela Pawlowska, et al., Exhausted T cell signature predicts immunotherapy response in ER-positive breast cancer. Nat Commun. 2020 Jul 17;11(1):3584. doi: 10.1038/s41467-020-17414-y.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#COMMUN#
33
#Nat#
37
#PD-L1#
37
#免疫特征#
0
#乳腺癌患者#
27
打卡
107