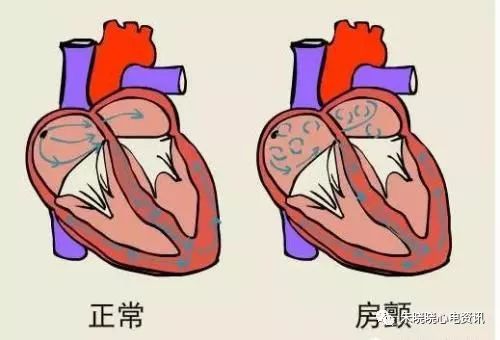
心房颤动在全球范围内的患病率和发病率都在增加,并导致许多不良结局,包括死亡率增加。肥胖是心房颤动的一个已知危险因素。超重和肥胖是继血压升高后心房颤动发病率的第二大因素,约占心房颤动病例的18%。此外,孟德尔随机研究结果提供的证据与BMI和心房颤动之间的因果关系一致。颈围增加是上身皮下脂肪的替代指标,与心血管风险和代谢风险因素相关。颈围与心房颤动之间的关联尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,当前研究的目的是评估颈围与心房颤动事件之间的关联。

研究人员从弗雷明汉心脏研究中选择了年龄≥55岁且未诊断为心房颤动且颈围、BMI和腰围测量值可用的参与者。根据Contal和O'Quigley变点法,研究人员将较大颈围定义为女性≥14英寸和男性≥17英寸。研究人员使用Fine-Gray模型来估计子分布风险比(sHRs),以评估颈围与心房颤动事件之间的关联,从而解释竞争性死亡风险。此外,研究人员调整了临床危险因素的模型。然后,研究人员分别调整了BMI、腰围和身高/体重。
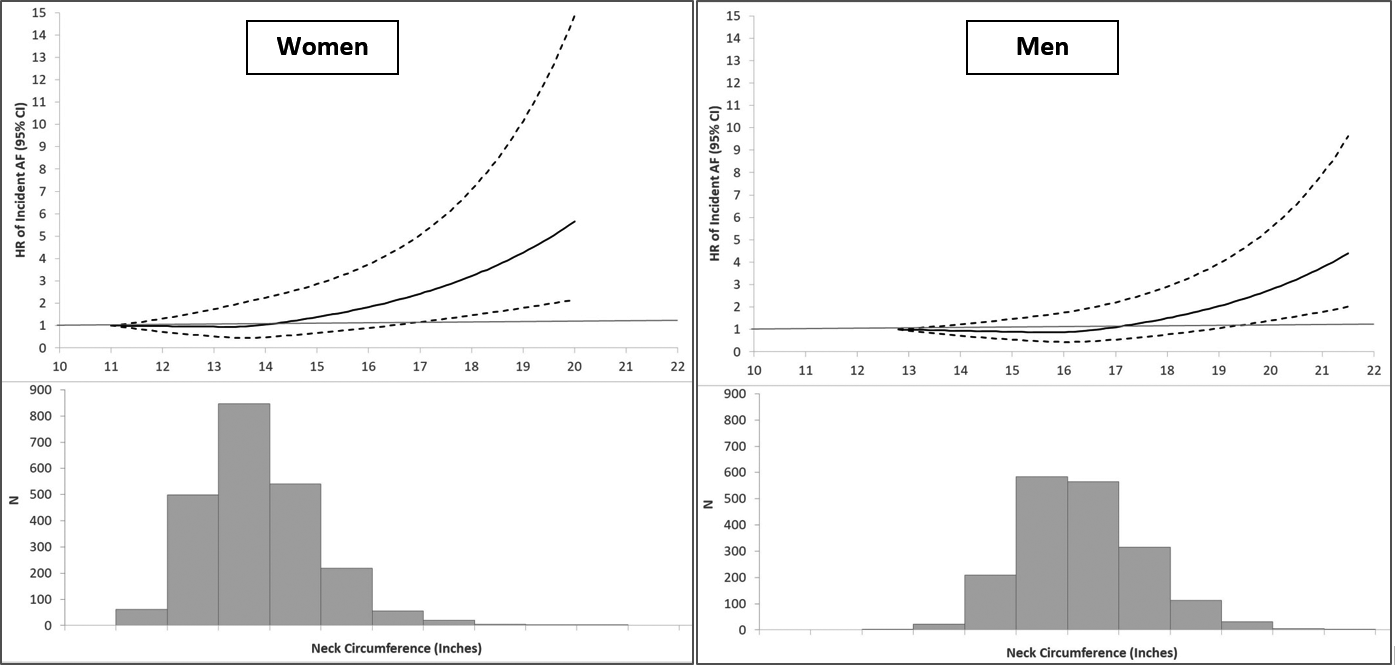
该研究样本纳入了4093名参与者(平均年龄为64±7岁,55%为女性)。在平均11.2±5.7年的随访期间,571名参与者发生了房颤事件。较大的颈围与发生心房颤动相关(较大与较小颈围相比的sHR为1.58;95%CI为1.32-1.90,P<0.0001)。在调整BMI(sHR为1.51;95%CI为1.21-1.89;P=0.0003)、腰围(sHR为1.47;95%CI为1.18-1.83;P<0.0001)和身高/体重后,该关联仍然显著(sHR为1.37;95%CI为1.09-1.72;P=0.007)。
由此可见,调整了传统的肥胖指标(如BMI和腰围)后,较大的颈围与心房颤动事件相关。
原始出处:
Jelena Kornej.et al.Neck Circumference and Risk of Incident Atrial Fibrillation in the Framingham Heart Study.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.022340
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#风险的关系#
72
#AHA#
59
#心房#
60
学系
70