Xerava(eravacycline)治疗复杂腹腔内感染:即将开展中国III期临床试验
2020-08-29 Allan MedSci原创
该公司完成了其Xerava(eravacycline)的III期临床试验的患者入组,用以治疗复杂腹腔内感染(cIAI)的中国患者。
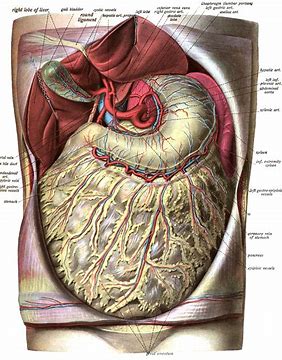
腹腔内感染通常由胃肠道的炎症或破裂引起。有时,腹腔感染也可来自泌尿道或女性生殖道。腹腔感染通常由多种微生物引起,可致腹腔脓肿或继发性腹膜炎,后者可能为广泛性,也可能为局限性(蜂窝织炎)。
生物制药公司Everest Medicines近日宣布,该公司完成了其Xerava(eravacycline)的III期临床试验的患者入组,用以治疗复杂腹腔内感染(cIAI)的中国患者。
Xerava(eravacycline)是一种新型、完全合成的广谱肠胃外四环素。在之前的两项全球关键研究中,Xerava在cIAI患者中具有良好的耐受性,并且与两种广泛使用的药物(ertapenem和meropenem)相比,在统计学上并不逊色。这两项研究导致Xerava在美国、欧盟和新加坡获得批准。这项中国试验的顶线结果预计将于2020年第四季度发布,并将支持Everest Medicines在中国提交新药申请。
Everest Medicines传染病首席医学官Sunny Zhu说:“我们的第一个中国III期临床试验是Everest Medicines的重要里程碑。Xerava代表着一种重要的新治疗方案,可用于处理复杂感染”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#I期临床#
21
#II期临床试验#
31
#III#
22
#腹腔内#
32
#腹腔内感染#
35
#ERA#
24
#I期临床试验#
22
#II期临床#
24
#III期临床试验#
19
#III期#
24