Hepatology:肝硬化患者骨髓情况研究
2016-08-05 Mechront 译 MedSci原创
背景和目的:骨髓(BM)免疫和造血细胞的储层,是组织修复和再生的关键。但是肝硬化患者所有这些功能都严重改变。我们的目的是探讨在肝硬化患者骨髓的细胞和功能状态。方法:研究了肝硬化患者(n = 168)和对照组(n = 44)的组织学、细胞和分子的变化。对造血干细胞(HSC)和相关小细胞、间充质干细胞(MSCs)、Schwann细胞、神经纤维和血管内皮细胞进行免疫组织化学研究。此外还对外周血和骨髓血浆
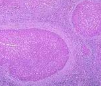
背景和目的:骨髓(BM)免疫和造血细胞的储层,是组织修复和再生的关键。但是肝硬化患者所有这些功能都严重改变。我们的目的是探讨在肝硬化患者骨髓的细胞和功能状态。
方法:研究了肝硬化患者(n = 168)和对照组(n = 44)的组织学、细胞和分子的变化。对造血干细胞(HSC)和相关小细胞、间充质干细胞(MSCs)、Schwann细胞、神经纤维和血管内皮细胞进行免疫组织化学研究。此外还对外周血和骨髓血浆中的细胞因子和生长因子进行了分析。
结果:肝硬化患者骨髓CD34+造血干细胞和MELD评分之间呈负相关(ρ=-0.582, p<0.001),和Child评分呈负相关(p<0.038)。肝硬化患者具有较高MELD (>15)的BMs与更低的MELD (≤15)相比,造血干细胞、MSCs、Schwann细胞和神经纤维显著增加,IL1β (p=0.004)、TNF-α (p=0.040)、IFN-γ (p=0.03)显著增加,抑瘤素M(p=0.04)、干细胞因子(SCF)(p=0.05)和基质细胞衍生因子(SDF-1)(p=0.03)显著下降。CD34细胞群体是脓毒症发展的预测(p<0.001),单位损失增加脓毒症的概率16%。肝硬化患者伴有较低的造血干细胞,与更低的血红蛋白(p= 0.05)和血小板计数(p= 0.05)有关,表明早期移植物功能障碍。
结论:日益严重的肝硬化引起造血龛紊乱和造血干细胞的损失,导致了血液和免疫障碍,减少潜在的再生。恢复骨髓功能可为肝硬化的治疗提供新的治疗选择。
原始出处:
Bihari C.et al.Bone Marrow Stem Cells and its Niche Components are Adversely Affected in Advanced Cirrhosis of Liver.Hepatology. 2016 Aug 3. doi: 10.1002/hep.28754. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












深度好文,值得学习
80
继续学习
78
继续关注
73
新话题
64
好文章,学习了
55
#EPA#
29
赞一个,学习好文章
30
恢复骨髓能治病,
34
肝硬化治疗上新的思路和突破
34
学习了,赞一个!!
34