CHEST:医生就比电脑牛!肺结节的良恶性还是医生评估的准!
2017-01-29 MedSci MedSci原创
肺结节的年发病率估计为157万。指南建议使用对恶性结节概率(pCA)的初步评估。以前的研究发现,尽管指南推荐这个建议,但是很多医生没有遵循指南。近期,一项发表在CHEST杂志上的文章研究了对肺结节诊断和检查的现状。此项研究基于最终诊断,对337例患者的肺结节的良恶属性分别进行医师评估(n=337)和此前确定的风险模型评估,并对两者进行比较。医师评估pCA分为低,中和高风险,并评估下一个诊断检查。研
肺结节的年发病率估计为157万。指南建议使用对恶性结节概率(pCA)的初步评估。以前的研究发现,尽管指南推荐这个建议,但是很多医生没有遵循指南。
此项研究基于最终诊断,对337例患者的肺结节的良恶属性分别进行医师评估(n=337)和此前确定的风险模型评估,并对两者进行比较。医师评估pCA分为低,中和高风险,并评估下一个诊断检查。
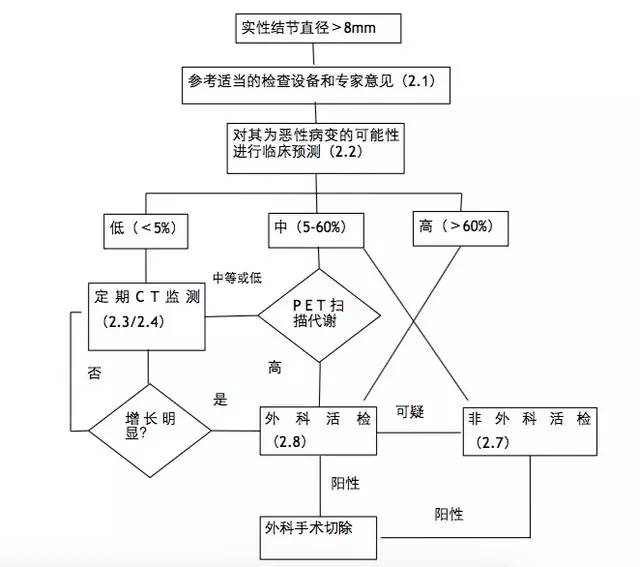
研究发现,一年内恶性肿瘤的发病率为47%(n=158)。医生评估的pCA优于结节预测计算器(AUC 0.85 vs.0.75,p<0.001和0.78,p=0.0001)。有61%的病例中选择下一个检查方法时(n=205),医生没有遵循指南的建议。尽管建议在具有低pCA的患者中进行连续CT成像,但是52%(n=13)的患者更积极地使用PET成像或活检;12%(n=3)的患者进行活检后为良性疾病。而在高风险类别中,大多数患者(n=103,75%)被更保守地管理。通过诊断分层,92%的(n=22)良性疾病患者进行更保守的CT扫描(20%),PET扫描(15%)或活检(8%),以及3例手术(8%)进行管理。
此项研究结果给表明:医师评估作为预测肺结节中恶性肿瘤的手段比先前验证的结节预测计算器更准确。尽管具有临床直觉的准确性,但是医生在选择下一个诊断检查时没有遵循基于指南的建议。为了提供最佳的患者护理,需要进行指南细化、实施和传播。
原始出处:
Tanner NT, Porter A, Gould M, et el. Physician assessment of pre-test probability of malignancy and adherence with guidelines for pulmonary nodule evaluation. Chest. 2017 Jan 20. pii: S0012-3692(17)30035-1. doi: 10.1016/j.chest.2017.01.018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EST#
35
#Chest#
31
謝謝分享
39
很好,不错,以后会多学习
49
长见识了
50
很有意义的文章,希望临床早日应用
51