患者开颅手术时唱歌,医生根据歌声卡顿避开语言功能区切脑瘤
2018-10-10 陆玫 通讯员 宋黎胜 澎湃新闻
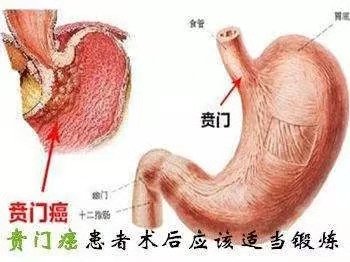
“海的思念绵延不绝,终于和天在地平线交会……”在浙江省人民医院日前进行的一台开颅手术中,25岁的患者小王(化名)清醒地唱着歌,医生则迅速切除贴近其大脑语言功能区的肿瘤。“我们根据患者的反应判断切除部位是否影响语言功能区——如果切除中歌声突然出现卡顿等变化,就说明碰到了功能区,要避开。”10月10日,该院神经外科副主任、主任医师楼林告诉记者,患者术后恢复良好,未出现语言障碍,11日就可出院。9月,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#开颅手术#
24
好
52
#脑瘤#
22
#语言#
29
#语言功能#
36
还是清醒状态下进行比较好
1