EClinicalMed:肠道菌群特征与社区获得性肺炎临床预后的相关性
2021-08-15 Nebula MedSci原创
肠道菌群和病毒群特征可能与社区获得性肺炎患者的临床预后有关
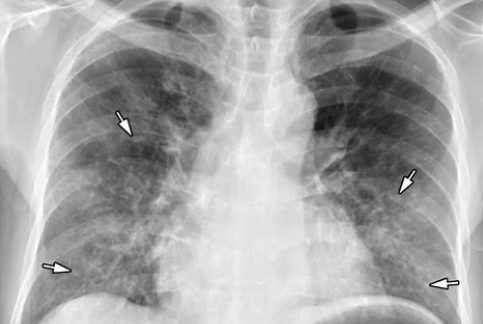
肠道菌群与免疫系统相互作用,可能有助于预防社区获得性肺炎(CAP)。肠道病毒与这些菌群紧密结合,但这些菌群在CAP患者中的组成及临床意义尚不清楚。
这项探索性研究的目的是在CAP患者住院期间表征直肠菌群和病毒群的组成,并确定微生物群特征是否与临床预后相关。
研究人员对2016年10月至2018年7月期间入住荷兰大学或社区医院的CAP患者和对照组进行了一项前瞻性观察队列研究。分别采用16S核糖体RNA基因测序和二代病毒发现测序对受试者的直肠细菌组和病毒组组成进行了分析。采用无监督多组因素分析评估细菌和病毒群落的共变异,作为主要预测因素。临床预后是病情稳定时间和住院时长。
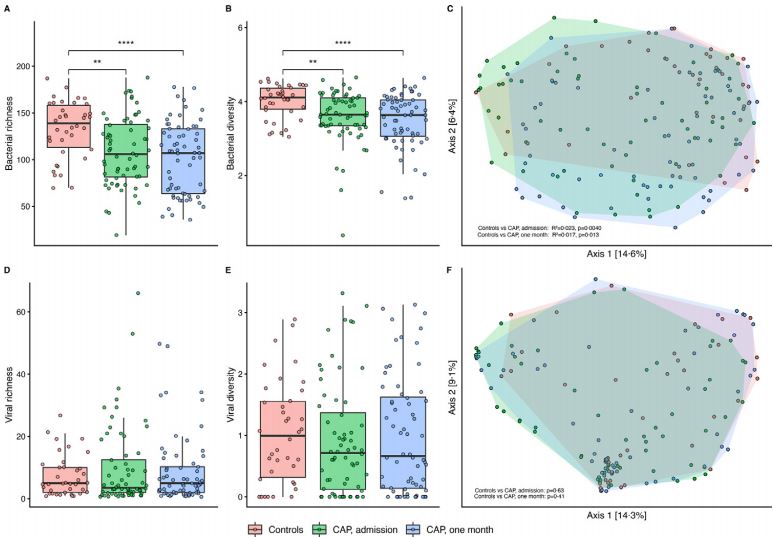
CAP患者和对照个体的肠道菌群丰度差异
共纳入了64位患者和38位对照。CAP患者的直肠细菌α (p=0.0015)和β多样性(r2=0.023, p=0.004)与对照组的不同。细菌和病毒的微生物群特征与临床病情稳定下来的时间(风险比[HR] 0.43, 95%CI 0.20-0.93, p=0.032)和住院时长(HR 0.37, 95CI 0.17-0.81, p=0.012)相关,虽然只有后者在检验多个候选切入点的p值调整后仍然显著(p值分别是0.12和0.046)。
细菌和病毒微生物群特征与CAP患者的临床预后的相关性
总之,这项探索性研究提供了初步证据,表明肠道菌群和病毒群特征可能与CAP患者的临床预后有关。在独立队列中验证这些探索性数据时,可以为基于微生物的诊断小组的发展提供信息,用于预测CAP患者的临床预估。
原始出处:
Robert F.J.Kullberg, et al. Rectal bacteriome and virome signatures and clinical outcomes in community-acquired pneumonia: An exploratory study. EClinicalMedicine. August 11, 2021. https://doi.org/10.1016/j.eclinm.2021.101074
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#获得性#
35
#相关性#
33
#肠道菌#
39
#社区#
42
#clinical#
28
#临床预后#
26
#Med#
32
很优秀,值得学习
66