Neurosurgery:诱导性高血压引起的 PRES
2019-09-25 杨中华 脑血管病及重症文献导读
诱导性高血压是治疗蛛网膜下腔出血(subarachnoid hemorrhage,SAH)后迟发性脑缺血(Delayed cerebral ischemia,DCI)的一种方法。
诱导性高血压是治疗蛛网膜下腔出血(subarachnoid hemorrhage,SAH)后迟发性脑缺血(Delayed cerebral ischemia,DCI)的一种方法。
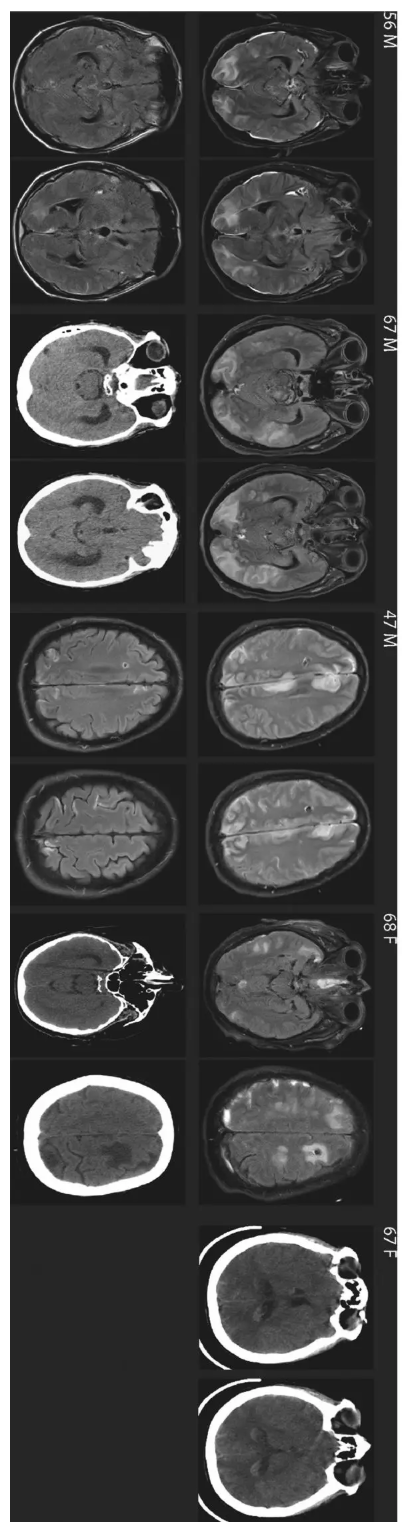
文献报道显示诱导性高血压会导致7%的患者发生可逆性后部脑病综合征(posterior reversible encephalopathy syndrome,PRES)。
下面5例患者为诱导性高血压引起的 PRES:
原始出处:
Michelle L Allen, et al. Posterior Reversible Encephalopathy Syndrome as a Complication of Induced Hypertension in Subarachnoid Hemorrhage: A Case-Control Study. Neurosurgery. 2019 Aug 1;85(2):223-230.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#surgery#
41
#诱导性高血压#
44
#GER#
37
#诱导性#
42
#ROS#
27
学习
68