Nat Med: II期临床试验: 黑色素瘤患者应该持续还是间歇给药?
2020-10-06 haibei MedSci原创
基于这些发现,研究人员前瞻性地测试了BRAF和MEK抑制剂联合的间歇性治疗与标准的每日连续给药相比是否能改善PFS。
BRAF和MEK抑制剂的联合治疗在晚期BRAFV600黑色素瘤患者中可以产生高达70%的客观响应率。然而,获得性耐药,通常由MAPK通路重新激活驱动,仍然十分常见。Das Thakur及其同事的临床前建模表明,在体外对BRAF抑制剂vemurafenib产生耐药的BRAFV600E细胞在没有药物的情况下生长不良。按照4周给药,2周停药的时间表间歇性地服用vemurafenib,在小鼠模型中延长了药物敏感性,增加了无进展生存期(PFS)。
在对BRAF和MEK抑制剂组合获得性耐药的BRAFV600突变细胞中,停药效果更加明显。
基于这些发现,研究人员前瞻性地测试了BRAF和MEK抑制剂联合的间歇性治疗与标准的每日连续给药相比是否能改善PFS。
最近,研究人员进行了S1320,一项随机、开放标签、II期临床试验(NCT02196181),来评估BRAF抑制剂达布拉非尼和MEK抑制剂曲美替尼的间歇性给药是否能改善转移性和不可切除的BRAFV600黑色素瘤患者的无进展生存。
患者在全国68个学术和社区站点入组。所有患者在8周的准备期内连续接受达布拉菲尼和曲美替尼治疗,之后,肿瘤无进展的患者随机接受这两种药物的连续或间歇性给药。其中,间歇性给药时间安排为3周停药,5周给药。
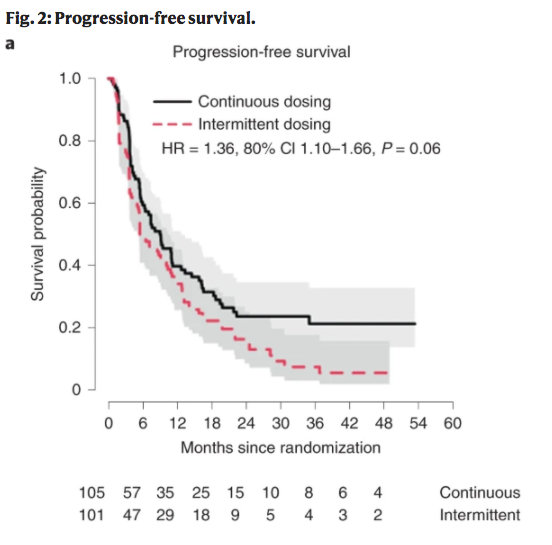
该试验已完成招募,206名基线特征相似的患者以1:1的比例随机分配到两个研究臂中(105人接受连续给药,101人接受间歇性给药)。
结果显示,与间歇性给药相比,持续给药产生了统计学意义上的随机化后无进展生存期的改善(中位数9.0个月对5.5个月,P = 0.064,预设两方α = 0.2)。
因此,与最初的假设相反,间歇性给药并没有改善患者的无进展生存期。在次要结果中,包括总生存期和治疗相关毒性的总发生率,两组之间没有差异。
原始出处:
Alain P. Algazi et al. Continuous versus intermittent BRAF and MEK inhibition in patients with BRAF-mutated melanoma: a randomized phase 2 trial. Nature Medicine (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#I期临床#
20
#Nat#
17
#II期临床试验#
35
#色素#
28
#I期临床试验#
0
#II期临床#
36
#黑色素#
16
#黑色素#
23
#Med#
31