J Clin Periodontol:运动减轻牙周炎大鼠牙槽骨吸收和焦虑行为
2017-10-29 MedSci MedSci原创
本实验目的为评估体育训练对Wistar大鼠牙周病(PD)的炎症和行为的影响。
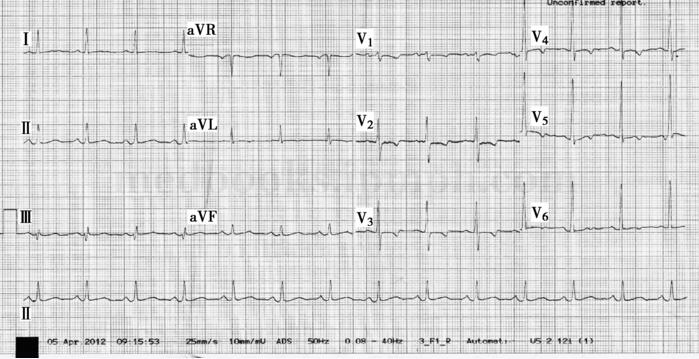
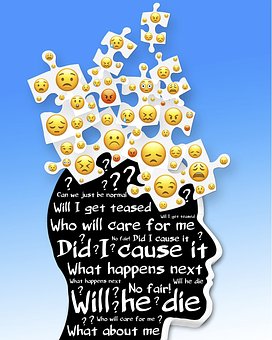
本实验目的为评估体育训练对Wistar大鼠牙周病(PD)的炎症和行为的影响。二十四只动物分布在2×2因子设计(有和没有运动,有和没有PD)。参与训练的动物在8周内每天游泳1小时。在实验结束前14天,通过结扎诱导PD,并且在最后一周,将所有动物进行Marble Burying Test。进行下颌骨的骨组织形态计量学分析及细胞因子表达的Western印迹法分析。我们还使用抗胶质纤维酸性蛋白抗体评估海马星形胶质细胞的形态测定。结果发现,身体训练使PD大鼠的骨吸收减轻和上皮附着水平丧失。患有PD的训练动物的牙周组织中TNF-α表达较低,而IL-10增加。训练有素的PD患者与诱导性牙周炎患者的TNF-α/ IL-10比值较低。 PD增加了患者的焦虑,而身体训练减弱了这一表现。运动增加没有PD的大鼠的海马星形胶质细胞。结论:运动减轻焦虑行为,炎症蛋白表达和PD大鼠的骨吸收。原始出处:Eric F. Andrade, et al. Exercise attenuates alveolar bone loss and anxiety-like behaviour in rats with period
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#牙槽骨#
27
#PE#
28
#牙槽骨吸收#
34
#牙周#
29
#骨吸收#
36