如何治疗系统性硬化症?候选药物GS248或提供临床益处
2021-01-28 Allan MedSci原创
制药公司Gesynta Pharma今天宣布,其候选药物GS-248的II期研究已入组了首批患者,预计将在2021年底完成这项临床试验。
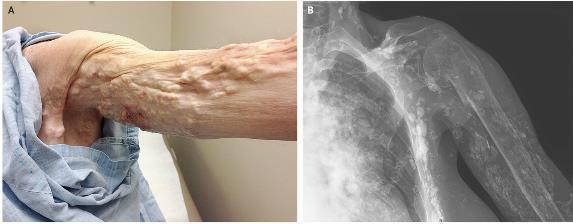
系统性硬化症是一种进行性自身免疫疾病,可导致对微血管的严重损害。在第一阶段,会导致手指和脚趾血流减少,进而引起疼痛并损害精细运动功能。在疾病过程的后期,患者处于手指溃疡和手指和/或脚趾伤口极度疼痛且难以愈合的危险中。由于微脉管系统的炎症,肺、肾和心脏也可能受到严重损害。
制药公司Gesynta Pharma今天宣布,其候选药物GS-248的II期研究已入组了首批患者,预计将在2021年底完成这项临床试验。候选药物GS-248能够选择性地抑制微粒体前列腺素E合酶1(mPGES-1),进而提供抗炎和血管舒张作用。一项I期研究表明,GS-248具有良好的药代动力学特性,可支持每日一次给药,并具有强大而持久的抗炎特性(PGE2降低)以及血管保护作用(前列环素增加)。
随机、安慰剂对照、双盲II期研究将在四个欧洲国家/地区纳入约80例患者。患者将每天一次口服GS-248或安慰剂,剂量为120 mg,持续4周。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#候选药物#
35
#硬化症#
34
#系统性#
33
双重疗效
88
#系统性硬化#
33