OCC 2020:伊伐布雷定改善心衰患者症状、心功能和生活质量!POSITIVE研究期中分析结果公布
2020-06-05 中国循环杂志 中国循环杂志
SHIFT试验表明伊伐布雷定可减慢心衰患者心率改善预后,真实世界又如何?
SHIFT试验表明伊伐布雷定可减慢心衰患者心率改善预后,真实世界又如何?
近日在第十四届东方心脏病会议心衰论坛上,大规模、前瞻性、观察性研究,慢性心衰患者应用伊伐布雷定的药品上市后有效性与安全性重点监测研究(POSITIVE研究)中期分析结果回答了这个问题。
POSITIVE的主要研究者和公布者,复旦大学附属中山医院的葛均波院士指出,“这项中国人群大规模的真实世界研究,也是首个亚洲最大样本量的有关伊伐布雷定的心衰领域真实世界研究。不仅对我国心衰患者的治疗方案有指导价值,对于亚洲其他国家也有借鉴意义”。
复旦大学附属中山医院的周京敏教授对POSITIVE研究中期分析进行了详细介绍,并指出,在标准临床治疗方案背景下应用伊伐布雷定可有效降低中国心衰患者的心率,改善症状、心功能和生活质量,且安全性和耐受性良好。
研究显示,接受伊伐布雷定治疗的心衰患者,在随访1个月和6个月时,心电图心率相对基线的变化分别为-13.2(95%CI:-15.2~ -11.8)次/分和-14.5(95%CI:-17.2~-11.8)次/分,各访视心率较基线变化均具有显著性统计学差异(P<0.001)。
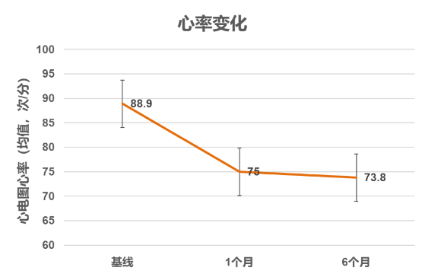
图1 接受伊伐布雷定治疗的慢性心衰患者在随访1个月和6个月时心电图心率相对基线的变化
此外,随访1个月和6个月时,生活质量问卷调查(KCCQ问卷)的临床症状得分和生活质量总得分情况总体均较基线增高,且差异均具有统计学意义(P<0.001)。
而且NYHA心功能分级显著改善,不同随访时间与基线期比较差异均有统计学意义(P均<0.001)。此外,左心室射血分数(LVEF)呈现提高趋势,B型利钠肽(BNP)/N末端B型利钠肽原(NT-proBNP)呈降低趋势。
慢性心衰患者应用伊伐布雷定也较为安全,共44例(6.7%)受试者报告了60起与研究药物相关的治疗后出现的不良事件,发生频率最高的是光幻视有6例(0.9%)、心动过缓6例(0.9%),与说明书描述的不良反应基本一致。
改善症状和生活质量是心衰管理的重要目标,既往发表的其他国家上市研究也同样提示伊伐布雷定有助于改善心衰患者症状和生活质量。
来自德国的INTENSIFY[1]研究发现,联合伊伐布雷定治疗4个月后,LVEF≤35%(26.6 vs 17.4%)及有心衰失代偿临床表现的患者比例均下降(22.7 vs 5.4%),EQ-5D生活质量评分提高。
同样是德国的RELIf-CHF[2]研究显示,随访12个月时,47%的基线有症状患者后续随访时症状消失,患者的EQ-5D和VAS评分亦得到改善。
英国的LIVE:LIFE研究[3]采用明尼苏达州心力衰竭生活调查问卷(MLWHFQ)评价生活质量,伊伐布雷定治疗6个月MLWHFQ总评分显著改善(降低9分,P<0.0001),身体和情感维度评分也显著改善。
OPTIMIZE优化心衰管理项目在全球多个国家开展,多项已发表的分析[4-6]表明出院前联合伊伐布雷定可优化心衰管理,改善患者症状、生活质量和心功能。
周京敏教授指出,POSITIVE研究基于中国临床实践,观察到伊伐布雷定有助于治疗和改善中国慢性心衰患者预后,且安全性良好。这些为优化心衰治疗方案提供了新证据和新思路。
这项POSITIVE研究中期分析,共纳入655例受试者,进入首次访视后1个月和6个月的受试者分别为554例(84.6%)和449例(68.5%)。平均年龄为(54.9±15.0)岁,男性占77.4%,平均心率为(88.9±12.4)次/分,心率80~100次/分的患者占55.7%,左室射血分数为(30.9±7.2)%,心力衰竭病程的中位时间为5.0个月,心力衰竭的主要原因为扩张型心肌病(299例,45.6%)和冠心病(237例,36.2%)。基线时83.1%的患者存在呼吸困难,78.8%的患者有乏力症状。
参考文献
[1]Adv Ther, 2014, 31(9): 961-974.
[2]Int J Cardiol, 2017, 240: 258-264.
[3]Int J Cardiol, 2017, 249: 313-318.
[4]Eur J Heart Fail, 2017,19 (Suppl. S1): 231.
[5]Int J Cardiol, 2018, 260:113-117.
[6]Int J Cardiol Heart Vasc, 2019, 22: 169-173.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#结果公布#
24
#SIT#
37
#OCC#
0
#心衰患者#
19
#OCC 2020#
38
#心功能#
34
#伊伐布雷定#
37